Pressure ulcers - what to ask your doctor
What to ask your doctor about pressure ulcers; Bedsores - what to ask your doctor
Pressure ulcers are also called bedsores, or pressure sores. They can form when your skin and soft tissue press against a harder surface, such as a chair or bed for a prolonged time. This pressure reduces the blood supply to that area. Lack of blood supply can cause the skin tissue in this area to become damaged or die. When this happens, a pressure ulcer may form.
Below are some questions you may want to ask your health care provider to help you or the person taking care of you to prevent and take care of pressure ulcers.
Prevent
Decubitus ulcer prevention; Bedsore prevention; Pressure sores prevention

Questions
Which parts of the body are more likely to get pressure sores?
- How often do these areas need to be looked at?
- What are the signs that a pressure ulcer is beginning to form?
What is the best way to take care of my skin every day?
- What types of lotions, creams, ointments, and powders are best to use?
- What type of clothing is best to wear?
What type of diet is best to prevent pressure ulcers or to help them heal?
When lying in bed:
- What positions are best when lying down?
- What types of padding or cushioning should I use?
- Should I use special mattresses or mattress covers? Sheets? Pajamas or other clothing?
- How often should I change my position?
- What is the best way to move or be moved around while I am in bed?
- What is the best way to transfer from bed to a wheelchair or chair?
If there is leakage of stool or urine, what else should be done to prevent pressure ulcers?
If using a wheelchair:
- How often should someone make sure the wheelchair is the right size?
- What type of cushions should I use?
- What is the best way to transfer into and out of the wheelchair?
- How often should I change position?
If a pressure ulcer or sore is present:
- What type of dressing should I use?
- How often does the dressing need to be changed?
- What are the signs that the ulcer is getting worse or is infected?
When should the doctor or nurse be called?
References
Witkowski JA, Parish LC, Campbell C, Parish JL. Decubitus ulcers. In: Lebwohl MG, Heymann WR, Berth-Jones J, Coulson I, eds. Treatment of Skin Disease: Comprehensive Therapeutic Strategies . 4th ed. Philadelphia, PA: Elsevier Saunders; 2014:chap 52.
-
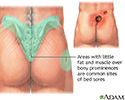
Areas where bedsores occur - illustration
Bedsores, also known as pressure sores or decubitus ulcers, are a breakdown and ulceration of tissue due to a combination of the weight of the body on the surface of the skin and the friction of a resistant surface such as a bed. Areas where bony prominences are less padded by muscle and fat, such as the hip bones, tailbone and heels of the feet, are most susceptible to bedsores. Non-mobile patients are vulnerable to the formation pressure sores when left lying for long periods of time in the same prone position.
Areas where bedsores occur
illustration
-
Areas where bedsores occur - illustration
Bedsores, also known as pressure sores or decubitus ulcers, are a breakdown and ulceration of tissue due to a combination of the weight of the body on the surface of the skin and the friction of a resistant surface such as a bed. Areas where bony prominences are less padded by muscle and fat, such as the hip bones, tailbone and heels of the feet, are most susceptible to bedsores. Non-mobile patients are vulnerable to the formation pressure sores when left lying for long periods of time in the same prone position.
Areas where bedsores occur
illustration
-
Peptic ulcers
(In-Depth)
-
Wounds
(Alt. Medicine)
-
Diabetes - type 2
(In-Depth)
-
Coronary artery disease
(In-Depth)
-
HIV and AIDS
(Alt. Medicine)
-
Licorice
(Alt. Medicine)
-
Pericarditis
(Alt. Medicine)
-
Reiter syndrome
(Alt. Medicine)
-
Tendinitis
(Alt. Medicine)
-
Raynaud's phenomenon
(Alt. Medicine)
- Preventing pressure ulcers
- How to care for pressure sores
- Skin flaps and grafts - self-care
- Diabetes - foot ulcers
- Diabetes - tests and checkups
- Diabetes - taking care of your feet
- Collateral ligament (CL) injury - aftercare
- Dislocated shoulder - aftercare
- Achilles tendon rupture - aftercare
- Shoulder separation - aftercare
Review Date: 5/17/2016
Reviewed By: Laura J. Martin, MD, MPH, ABIM Board Certified in Internal Medicine and Hospice and Palliative Medicine, Atlanta, GA. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.