Leg amputation - discharge
Amputation - leg - discharge; Below knee amputation - discharge; BK amputation - discharge; Above knee - discharge; AK - discharge; Trans-femoral amputation - discharge; Trans-tibial amputation - discharge
What Happened in the Hospital
You have had all or part of your leg amputated. You may have had an accident, or your leg may have had a blood clot, infection, or disease, and doctors could not save it.
What to Expect at Home
You may feel sad, angry, frustrated and depressed. All of these feelings are normal and may arise in the hospital or when you get home.
It will take time for you to learn to use a walker, and a wheelchair. It will also take time to learn to get in and out of the wheelchair.
You may be getting a prosthesis , a man-made limb to replace your limb that was removed. It will take time for your prosthesis to be made. When you have it, getting used to it will also take time.
Prosthesis
A prosthesis is a device designed to replace a missing part of the body or to make a part of the body work better. Diseased or missing eyes, arms, h...

You may have pain in your limb for several days after your surgery. You may also have a feeling that your limb is still there. This is called phantom sensation .
Self-care
Family and friends can help. Talking with them about your feelings may make you feel better. They can also help you do things around your house and when you go out.
If you feel sad or depressed, ask your health care provider about seeing a mental health counselor for help with your feelings about your amputation.
If you have diabetes, keep your blood sugar in good control .
Keep your blood sugar in good control
Hyperglycemia - control; Hypoglycemia - control; Diabetes - blood sugar control; Blood glucose - managing

If you have poor blood flow, follow your provider's instructions for diet and medicines. Your provider may give you medicines for your pain.
You may eat your normal foods when you get home.
Activity
Do things that will help you get stronger and do your daily activities, such as bathing and cooking. You should try to do as much as possible on your own.
When you are sitting, keep your stump straight and level. You can put your stump on a padded board to keep it straight when you are sitting. You can also lie on your belly to make sure your leg is straight. This can help keep your joints from getting stiff.
Try not to turn your stump in or out when you are lying in bed or sitting in a chair. You can use rolled up towels or blankets next to your legs to keep them in line with your body.
DO NOT cross your legs when you are sitting. It can stop the blood flow to your stump.
You may raise up the foot of your bed to keep your stump from swelling and to help ease pain. DO NOT place a pillow under your stump.
Wound and Stump Care
Keep your wound clean and dry unless your provider tells you it is OK to get it wet. Clean the area around the wound gently with mild soap and water. DO NOT rub the incision. Allow water to flow gently over it. DO NOT take a bath or swim.
After your wound is healed, keep it open to the air unless a provider or nurse tells you something different. After dressings have been removed , wash your stump daily with mild soap and water. DO NOT soak it. Dry it well.
After dressings have been removed
No definition available for this article.
Inspect your stump everyday. Use a mirror if it is hard for you to see all around it. Look for any red areas or dirt.
Wear your elastic bandage all the time. Rewrap it every 2 to 4 hours. Make sure there are no creases in it. Wear your stump protector whenever you are out of bed.
Ask your provider for help with pain. Two things that may help are:
- Tapping along the scar and in small circles along the stump, if that is not painful
- Rubbing the scar and stump gently with linen or soft cotton
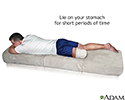
Lie on your stomach 3 or 4 times a day for about 20 minutes. This will stretch out your hip muscle. If you had a below-the-knee amputation, you may put a pillow behind your calf to help straighten your knee.
Practice transfers at home.
-
Go from your
bed to your wheelchair
, a chair, or the toilet.
Bed to your wheelchair
Pivot turn; Transfer from bed to wheelchair
Read Article Now Book Mark Article - Go from a chair to your wheelchair.
- Go from your wheelchair to the toilet.
Stay as active with your walker as you can.
Ask your provider for advice about how to avoid constipation .
Avoid constipation
Constipation is when you do not pass stool as often as you normally do. Your stool becomes hard and dry, and it is difficult to pass. You might fee...
When to Call the Doctor
Call your provider if:
- Your stump looks redder or there are red streaks on your skin going up your leg
- Your skin feels warmer to touch
- There is swelling or bulging around the wound
- There is new drainage or bleeding from the wound
- There are new openings in the wound, or the skin around the wound is pulling away
- Your temperature is above 101.5°F (38.6°C) more than once
- Your skin around the stump or wound is dark or it is turning black
- Your pain is worse and your pain medicines are not controlling it
- Your wound has gotten larger
- A foul smell is coming from the wound
References
Department of Veterans Affairs, Department of Defense. VA/DOD Clinical Practice Guideline for Management for Rehabilitation of Lower Limb Amputation. Updated January 2008. www.healthquality.va.gov/amputation/amp_sum_508.pdf . Accessed July 1, 2014.
Mihalko MJ. Amputations of the Lower Extremity. In: Canale ST, Beaty JH, eds. Campbell's Operative Orthopaedics . 12th ed. Philadelphia, PA: Elsevier Mosby; 2013:chap 16.
Toy PC. General Principles of Amputations. In: Canale ST, Beaty JH, eds. Campbell's Operative Orthopaedics . 12th ed. Philadelphia, PA: Elsevier Mosby; 2013:chap 14.
-
Stump care - illustration
Lie on your stomach 3 or 4 times a day for about 20 minutes. Lying on your stomach will help stretch out your hip muscle.
Stump care
illustration
Review Date: 4/17/2016
Reviewed By: C. Benjamin Ma, MD, Assistant Professor, Chief, Sports Medicine and Shoulder Service, UCSF Department of Orthopaedic Surgery. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.