Skin care and incontinence
Incontinence - skin care; Incontinence - pressure sore; Incontinence - pressure ulcer
Information
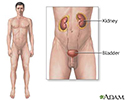
People who have problems controlling their urine or bowels (called incontinence) are at risk of skin problems. Skin areas most affected are near the buttocks, hips, genitals, and between the pelvis and rectum (perineum).
Urine
Urinary (or bladder) incontinence happens when you are not able to keep urine from leaking out of your urethra. The urethra is the tube that carries...

Bowels
Bowel incontinence is the loss of bowel control, causing you to pass stool unexpectedly. This can range from sometimes leaking a small amount of sto...

Excess moisture in these areas makes skin problems such as redness, peeling, irritation, and yeast infections likely.
Yeast infections
Candida infection of the skin is a yeast infection of the skin. The medical name of the condition is cutaneous candidiasis.

Bedsores ( pressure sores ) may also develop if the person:
Pressure sores
Pressure ulcer - care; Bedsore - care; Decubitus ulcer - care
-
Has not been eating well (is
malnourished
)
Malnourished
Malnutrition is the condition that occurs when your body does not get enough nutrients.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Received
radiation therapy
to the area
Radiation therapy
Radiation therapy uses high-powered x-rays, particles, or radioactive seeds to kill cancer cells.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Spends most or all of the day in a wheelchair, regular chair, or bed without changing position
TAKING CARE OF THE SKIN
Using diapers and other products can make skin problems worse. Although they may keep bedding and clothing cleaner, these products allow urine or stool to be in constant contact with the skin. Over time, the skin breaks down. Special care must be taken to keep the skin clean and dry. This can be done by:
- Cleaning and drying the area right away after urinating or having a bowel movement.
- Cleaning the skin with mild, dilute soap and water then rinsing well and gently patting dry.
Use soap-free skin cleansers that do not cause dryness or irritation. Follow the product's instructions. Some products do not require rinsing.
Moisturizing creams can help keep the skin moist. Avoid products that contain alcohol, which may irritate the skin. If you are receiving radiation therapy, ask your health care provider if it is OK to use any creams or lotions.
Consider using a skin sealant or moisture barrier. Creams or ointments that contain zinc oxide, lanolin, or petrolatum form a protective barrier on the skin. Some skin care products, often in the form of a spray or a towelette, create a clear, protective film over the skin. A provider can recommend barrier creams to help protect the skin.
Even if these products are used, the skin must still be cleaned each time after passing urine or stool. Reapply the cream or ointment after cleaning and drying the skin.
Incontinence problems can cause a yeast infection on the skin. This is an itchy, red, pimple-like rash. The skin may feel raw. Products are available to treat a yeast infection:
- If the skin is moist most of the time, use a powder with antifungal medicine, such as nystatin or miconazole. DO NOT use baby powder.
- A moisture barrier or skin sealant may be applied over the powder.
- If severe skin irritation develops, see the provider.
- If bacterial infection occurs, antibiotics applied to the skin or taken by mouth may help.
The National Association for Continence (NAFC) helpful information at www.nafc.org .
IF THE PERSON IS BEDRIDDEN OR USING A WHEELCHAIR
Check the skin for pressure sores every day. Look for reddened areas that do not turn white when pressed. Also look for blisters, sores, or craters. Tell the provider if there is any foul-smelling drainage.
A healthy, well-balanced diet that contains enough calories and protein helps keep the person healthy.
For people who must stay in bed:
- Have them change position often, at least every 2 hours
- Change sheets and clothing right away after they are soiled
- Use items that can help reduce pressure, such as pillows or foam padding
For people in a wheelchair:
- Make sure the chair fits properly
- Have them shift their weight every 15 to 20 minutes
- Use items that can help reduce pressure, such as pillows or foam padding
A well-balanced diet that contains enough calories and protein helps keep the person healthy. Also, smoking affects healing of the skin, so stopping smoking is important.
References
Holroyd S. Incontinence-associated dermatitis: identification, prevention and care. Br J Nurs . 2015;24(9):S37-S38. PMID: 25978474 www.ncbi.nlm.nih.gov/pubmed/25978474 .
Jacobson TM, Wright T. Improving quality by taking aim at incontinence-associated dermatitis in hospitalized adults. Medsurg Nurs . 2015;24(3):151-157. PMID: 26285369 www.ncbi.nlm.nih.gov/pubmed/26285369 .
Markland AD. Constipation and fecal incontinence. In: Ham RJ, Sloane PD, Warshaw GA, Potter JF, Flaherty E, eds. Ham's Primary Care Geriatrics: A Case-Based Approach . 6th ed. Philadelphia, PA: Elsevier Saunders; 2014:chap 24.
Review Date: 1/31/2016
Reviewed By: Kevin Berman, MD, PhD, Atlanta Center for Dermatologic Disease, Atlanta, GA. Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.