Lung surgery
Thoracotomy; Lung tissue removal; Pneumonectomy; Lobectomy; Lung biopsy; Thoracoscopy; Video-assisted thoracoscopic surgery; VATS
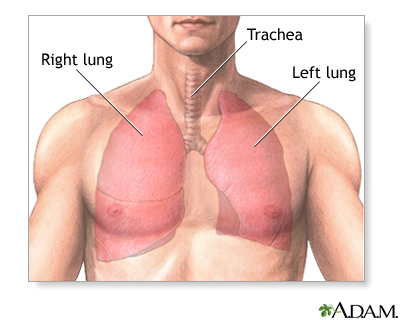
Lung surgery is surgery done to repair or remove lung tissue. There are many common lung surgeries, including:
- Biopsy of an unknown growth
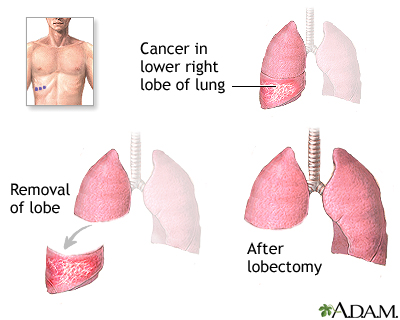
- Lobectomy, to remove one or more lobes of a lung
- Lung transplant
- Pneumonectomy, to remove a lung
- Surgery to prevent the buildup or return of fluid to the chest (pleurodesis)
-
Surgery to remove an infection in the chest cavity (
empyema
)
Empyema
Empyema is a collection of pus in the space between the lung and the inner surface of the chest wall (pleural space).
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Surgery to remove blood in the chest cavity, particularly after trauma
-
Surgery to remove small balloon-like tissues (blebs) that cause lung collapse (
pneumothorax
)
Pneumothorax
A collapsed lung occurs when air escapes from the lung. The air then fills the space outside of the lung, between the lung and chest wall. This bui...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Wedge resection, to remove part of a lobe in a lung
A thoracotomy is a surgical cut that a surgeon makes to open the chest wall.
Description
You will have general anesthesia before surgery. You will be asleep and unable to feel pain. Two common ways to do surgery on your lungs are thoracotomy and video-assisted thoracoscopic surgery (VATS). Robotic surgery may also be used.
General anesthesia
General anesthesia is treatment with certain medicines that puts you into a deep sleep so you do not feel pain during surgery. After you receive the...
Lung surgery using a thoracotomy is called open surgery. In this surgery:
- You will lie on your side on an operating table. Your arm will be placed above your head.
- Your surgeon will make a surgical cut between two ribs. The cut will go from the front of your chest wall to your back, passing just underneath the armpit. These ribs will be separated or a rib may be removed.
- Your lung on this side will be deflated so that air will not move in and out of it during surgery. This makes it easier for the surgeon to operate on the lung.
- Your surgeon may not know how much of your lung needs to be removed until your chest is open and the lung can be seen.
- Your surgeon may also remove lymph nodes in this area.
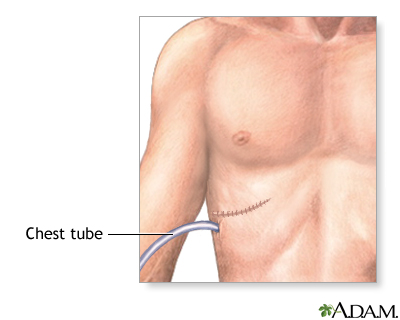
- After surgery, one or more drainage tubes will be placed into your chest area to drain out fluids that build up. These tubes are called chest tubes.
- After the surgery on your lung, your surgeon will close the ribs, muscles, and skin with sutures.
- Open lung surgery may take from 2 to 6 hours.
Video-assisted thoracoscopic surgery:
- Your surgeon will make several small surgical cuts over your chest wall. A videoscope (a tube with a tiny camera on the end) and other small tools will be passed through these cuts.
- Then, your surgeon may remove part or all of your lung, drain fluid or blood that has built up, or do other procedures.
- One or more tubes will be placed into your chest to drain fluids that build up.
- This procedure leads to much less pain and a faster recovery than open lung surgery.
Why the Procedure Is Performed
Thoracotomy or video-assisted thoracoscopic surgery may be done to:
-
Remove
cancer
(such as
lung cancer
) or biopsy an unknown growth
Cancer
Cancer is the uncontrolled growth of abnormal cells in the body. Cancerous cells are also called malignant cells.
Read Article Now Book Mark ArticleLung cancer
Small cell lung cancer (SCLC) is a fast-growing type of lung cancer. It spreads much more quickly than non-small cell lung cancer. There are two typ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Treat injuries that cause lung tissue to collapse (
pneumothorax
or
hemothorax
)
Pneumothorax
A collapsed lung occurs when air escapes from the lung. The air then fills the space outside of the lung, between the lung and chest wall. This bui...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleHemothorax
Hemothorax is a collection of blood in the space between the chest wall and the lung (the pleural cavity).
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Treat permanently
collapsed lung
tissue (
atelectasis
)
Collapsed lung
A collapsed lung occurs when air escapes from the lung. The air then fills the space outside of the lung, between the lung and chest wall. This bui...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleAtelectasis
Atelectasis is the collapse of part or, much less commonly, all of a lung.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Remove lung tissue that is diseased or damaged from emphysema or
bronchiectasis
Bronchiectasis
Bronchiectasis is a disease in which the large airways in the lungs are damaged. This causes the airways to become wider. Bronchiectasis can be pres...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Remove blood or blood clots (
hemothorax
)
Hemothorax
Hemothorax is a collection of blood in the space between the chest wall and the lung (the pleural cavity).
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Remove tumors, such as
solitary pulmonary nodule
Solitary pulmonary nodule
A solitary pulmonary nodule is a round or oval spot (lesion) in the lung that is seen with a chest x-ray or CT scan.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Inflate
lung tissue that has collapsed
(This may be due to disease such as chronic obstructive pulmonary disease, or an injury.)
Lung tissue that has collapsed
A collapsed lung occurs when air escapes from the lung. The air then fills the space outside of the lung, between the lung and chest wall. This bui...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Remove infection in the chest cavity (empyema)
- Stop fluid buildup in the chest cavity (pleurodesis)
-
Remove a blood clot from the pulmonary artery (
pulmonary embolism
)
Pulmonary embolism
A pulmonary embolus is a blockage of an artery in the lungs. The most common cause of the blockage is a blood clot.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Treat complications of tuberculosis
Video-assisted thoracoscopic surgery can be used to treat many of these conditions. In some cases, video surgery may not be possible, and the surgeon may have to switch to an open surgery.
Risks
Risks of this surgery include:
- Failure of the lung to expand
- Injury to the lungs or blood vessels
- Need for a chest tube after surgery
- Pain
- Prolonged air leak
- Repeated fluid buildup in the chest cavity
- Bleeding
- Infection
- Heart rhythm disturbances
- Damage to the diaphragm, esophagus, or trachea
- Death
Before the Procedure
You will have several visits with your health care provider and undergo medical tests before your surgery. Your provider will:
- Do a complete physical exam
-
Make sure other medical conditions you may have, such as
diabetes
,
high blood pressure
, or heart or lung problems are under control
Diabetes
Diabetes is a chronic disease in which the body cannot regulate the amount of sugar in the blood.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleHigh blood pressure
Blood pressure is a measurement of the force exerted against the walls of your arteries as your heart pumps blood to your body. Hypertension is the ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Perform tests to make sure that you will be able to tolerate the removal of your lung tissue, if necessary
If you are a smoker, you should stop smoking several weeks before your surgery. Ask your provider for help.
Stop smoking
There are many ways to quit smoking. There are also resources to help you. Family members, friends, and co-workers may be supportive. But to be su...

Always tell your provider:
- Which drugs, vitamins, herbs, and other supplements you are taking, even ones you bought without a prescription
- If you have been drinking a lot of alcohol, more than 1 or 2 drinks a day
During the week before your surgery:
- You may be asked to stop taking drugs that make it hard for your blood to clot. Some of these are aspirin, ibuprofen (Advil, Motrin), vitamin E, warfarin (Coumadin), clopidogrel (Plavix), or ticlopidine (Ticlid).
- Ask your provider which drugs you should still take on the day of your surgery.
- Prepare your home for your return from the hospital.
On the day of your surgery:
- Do not eat or drink anything after midnight the night before your surgery.
- Take the medicines your doctor prescribed with small sips of water.
- Your provider will tell you when to arrive at the hospital.
After the Procedure
Most people stay in the hospital for 5 to 7 days after open thoracotomy. Hospital stay for a video-assisted thoracoscopic surgery is most often shorter. You may spend time in the intensive care unit (ICU) after either surgery.
During your hospital stay, you will:
- Be asked to sit on the side of the bed and walk as soon as possible after surgery.
- Have tube(s) coming out of the side of your chest to drain fluids and air.
- Wear special stockings on your feet and legs to prevent blood clots.
- Receive shots to prevent blood clots.
- Receive pain medicine through an IV (a tube that goes into your veins) or by mouth with pills. You may receive your pain medicine through a special machine that gives you a dose of pain medicine when you push a button. This allows you to control how much pain medicine you get. You may also have an epidural placed. This is a catheter in the back that delivers pain medicine to numb the nerves to the surgical area.
- Be asked to do a lot of deep breathing to help prevent pneumonia and infection. Deep breathing exercises also help inflate the lung that was operated on. Your chest tube(s) will remain in place until your lung has fully inflated.
Outlook (Prognosis)
The outcome depends on:
- The type of problem being treated
- How much lung tissue (if any) is removed
- Your overall health before surgery
References
Alfille PH, Wiener-Kronish JP, Bagchi A. Preoperative evaluation. In: Broaddus VC, Mason RJ, Ernst JD, et al, eds. Murray & Nadel's Textbook of Respiratory Medicine . 6th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 27.
Feller-Kopman DJ, Decamp MM. Interventional and surgical approaches to lung disease. In: Goldman L, Schafer AI, eds. Goldman's Cecil Medicine. 25th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 101.
Putnam JB. Lung, chest wall, pleura, and mediastinum. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery . 20th ed. Philadelphia, PA: Elsevier Saunders; 2017:chap 57.
Review Date: 5/24/2016
Reviewed By: Mary C. Mancini, MD, PhD, Department of Surgery, Louisiana State University Health Sciences Center-Shreveport, Shreveport, LA. Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.