Severe acute respiratory syndrome (SARS)
SARS
Severe acute respiratory syndrome (SARS) is a serious form of pneumonia . It is caused by a virus that was first identified in 2003. Infection with the SARS virus causes acute respiratory distress (severe breathing difficulty) and sometimes death.
Pneumonia
Pneumonia is a breathing (respiratory) condition in which there is an infection of the lung. This article covers community-acquired pneumonia (CAP). ...

Acute
Acute means sudden or severe. Acute symptoms appear, change, or worsen rapidly. It is the opposite of chronic.

Causes
SARS is caused by a member of the coronavirus family of viruses (the same family that can cause the common cold ). It is believed the 2003 epidemic started when the virus spread from small mammals in China.
Common cold
The common cold most often causes a runny nose, nasal congestion, and sneezing. You may also have a sore throat, cough, headache, or other symptoms....

When someone with SARS coughs or sneezes, infected droplets spray into the air. You can catch the SARS virus if you breathe in or touch these particles. The SARS virus may live on hands, tissues, and other surfaces for up to 6 hours in these droplets and up to 3 hours after the droplets have dried.
While the spread of droplets through close contact caused most of the early SARS cases, SARS might also spread by hands and other objects the droplets has touched. Airborne transmission is a real possibility in some cases. Live virus has even been found in the stool of people with SARS, where it has been shown to live for up to 4 days. The virus may be able to live for months or years when the temperature is below freezing.
With other coronaviruses, becoming infected and then getting sick again (re-infection) is common. This may also be the case with SARS.
Symptoms usually occur about 2 to 10 days after coming in contact with the virus. In some cases, SARS started sooner or later after first contact. People with active symptoms of illness are contagious. But it is not known for how long a person may be contagious before or after symptoms appear.
Symptoms
The main symptoms are:
- Cough
- Difficulty breathing
- Fever greater than 100.4°F (38.0°C)
- Other breathing symptoms
The most common symptoms are:
- Chills and shaking
- Cough, usually starts 2 to 3 days after other symptoms
- Fever
- Headache
- Muscle aches
Less common symptoms include:
- Cough that produces phlegm (sputum)
- Diarrhea
- Dizziness
- Nausea and vomiting
- Runny nose
- Sore throat
In some people, the lung symptoms get worse during the second week of illness, even after the fever has stopped.
Exams and Tests
Your health care provider may hear abnormal lung sounds while listening to your chest with a stethoscope. In most people with SARS, a chest x-ray or chest CT show pneumonia, which is typical with SARS.
Chest CT
A chest CT (computed tomography) scan is an imaging method that uses x-rays to create cross-sectional pictures of the chest and upper abdomen....

Tests used to diagnose SARS might include:
- Arterial blood tests
- Blood clotting tests
-
Blood chemistry tests
Blood chemistry tests
A comprehensive metabolic panel is a group of blood tests. They provide an overall picture of your body's chemical balance and metabolism. Metaboli...
Read Article Now Book Mark Article - Chest x-ray or chest CT scan
-
Complete blood count
(CBC)
Complete blood count
A complete blood count (CBC) test measures the following:The number of red blood cells (RBC count)The number of white blood cells (WBC count)The tota...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Tests used to quickly identify the virus that causes SARS include:
-
Antibody
tests for SARS
Antibody
An antibody is a protein produced by the body's immune system when it detects harmful substances, called antigens. Examples of antigens include micr...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Direct isolation of the SARS virus
- Rapid polymerase chain reaction (PCR) test for SARS virus
All current tests have some limitations. They may not be able to easily identify a SARS case during the first week of the illness, when it is most important.
Treatment
People who are thought to have SARS should be checked right away by a provider. If they are suspected of having SARS, they should be kept isolated in the hospital.
Treatment may include:
- Antibiotics to treat bacteria that cause pneumonia
- Antiviral medicines (although how well they work for SARS is unknown)
- High doses of steroids to reduce swelling in the lungs (it is not known how well they work)
- Oxygen, breathing support (mechanical ventilation), or chest therapy
In some serious cases, the liquid part of blood from people who have already recovered from SARS has been given as a treatment.
There is no strong evidence that these treatments work well. There is evidence that the antiviral medicine, ribavirin, does not work.
Outlook (Prognosis)
The death rate from SARS was 9 to 12% of those diagnosed. In people over age 65, the death rate was higher than 50%. The illness was milder in younger people.
Many more people became sick enough to need breathing assistance. And even more people had to go to hospital intensive care units.
Public health policies have been effective at controlling outbreaks. Many nations have stopped the epidemic in their own countries. All countries must continue to be careful to keep this disease under control. Viruses in the coronavirus family are known for their ability to change (mutate) in order to spread among humans.
Possible Complications
Complications may include:
- Respiratory failure
- Liver failure
- Heart failure
When to Contact a Medical Professional
Call your health care provider if you or someone you have been in close contact with someone who has SARS.
Prevention
Reducing your contact with people who have SARS lowers your risk for the disease. Avoid travel to places where there is an uncontrolled SARS outbreak. When possible, avoid direct contact with people who have SARS until at least 10 days after their fever and other symptoms are gone.
- Hand hygiene is the most important part of SARS prevention. Wash your hands or clean them with an alcohol-based instant hand sanitizer.
- Cover your mouth and nose when you sneeze or cough. Droplets that are released when a person sneezes or coughs are infectious.
- DO NOT share food, drink, or utensils.
- Clean commonly touched surfaces with an EPA-approved disinfectant.
Masks and goggles may be useful for preventing the spread of the disease. You may use gloves when handling items that may have touched infected droplets.
References
Gerber SI, Anderson LJ. Coronaviruses. In: Goldman L, Schafer AI, eds. Goldman's Cecil Medicine . 25th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 366.
McIntosh K, Perlman S. Coronaviruses, including severe acute respiratory distress syndrome (SARS)and Middle East respiratory syndrome (MERS). In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Disease . 8th ed. Philadelphia, PA: Elsevier Saunders; 2015:chap 157.
-
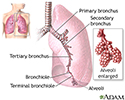
Lungs - illustration
The major features of the lungs include the bronchi, the bronchioles and the alveoli. The alveoli are the microscopic blood vessel-lined sacks in which oxygen and carbon dioxide gas are exchanged.
Lungs
illustration
-
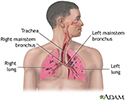
Respiratory system - illustration
Air is breathed in through the nasal passageways, travels through the trachea and bronchi to the lungs.
Respiratory system
illustration
-
Lungs - illustration
The major features of the lungs include the bronchi, the bronchioles and the alveoli. The alveoli are the microscopic blood vessel-lined sacks in which oxygen and carbon dioxide gas are exchanged.
Lungs
illustration
-
Respiratory system - illustration
Air is breathed in through the nasal passageways, travels through the trachea and bronchi to the lungs.
Respiratory system
illustration
-
Pneumonia
(In-Depth)
-
Chronic obstructive pulmonary disease
(In-Depth)
-
Sinusitis
(In-Depth)
-
Common cold
(Alt. Medicine)
-
Sickle cell disease
(In-Depth)
-
Restless legs syndrome and related disorders
(In-Depth)
-
Ear infections
(In-Depth)
-
Scleroderma
(In-Depth)
-
Otitis media
(Alt. Medicine)
-
Asthma in adults
(In-Depth)
Review Date: 2/2/2015
Reviewed By: Denis Hadjiliadis, MD, MHS, Paul F. Harron Jr. Associate Professor of Medicine, Pulmonary, Allergy, and Critical Care, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.