Meckel diverticulectomy
Meckel diverticulectomy; Meckel diverticulum - surgery; Meckel diverticulum - repair; GI bleeding - Meckel diverticulectomy; Gastrointestinal bleeding - Meckel diverticulectomy
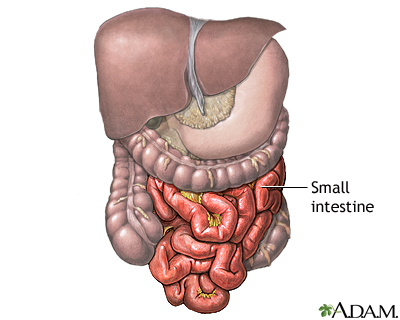
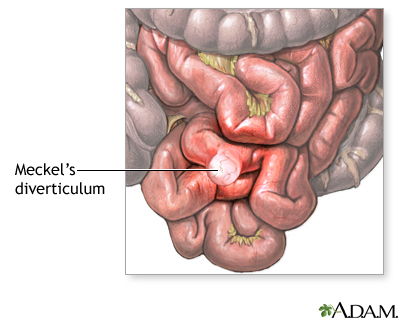
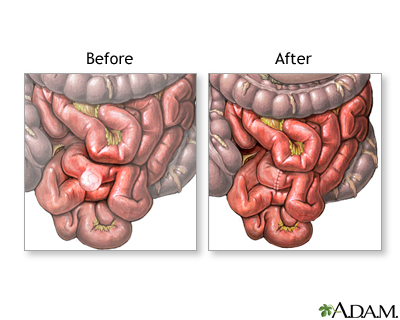
Meckel diverticulectomy is surgery to remove an abnormal pouch on the lining of the small intestine (bowel). This pouch is called a Meckel diverticulum .
Meckel diverticulum
A Meckel diverticulum is a pouch on the wall of the lower part of the small intestine that is present at birth (congenital). The diverticulum may co...

Description
You will receive general anesthesia before surgery. This will make you sleep and unable to feel pain.
General anesthesia
General anesthesia is treatment with certain medicines that puts you into a deep sleep so you do not feel pain during surgery. After you receive the...
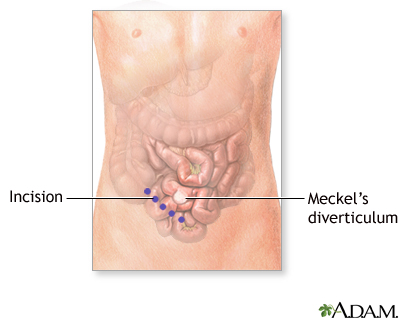
If you have open surgery:
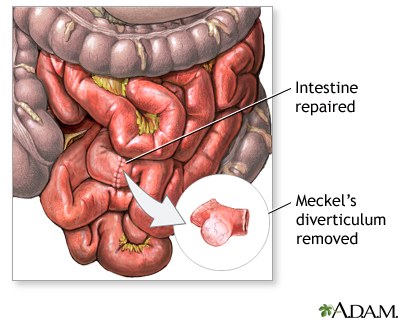
- Your surgeon will make a large surgical cut in your belly to open up the area.
- Your surgeon will look at the small intestine in the area where the pouch or diverticulum is located.
- Your surgeon will remove the diverticulum from the wall of your intestine.
-
Sometimes, the surgeon may need to remove a small part of your intestine along with the diverticulum. If this is done, the open ends of your intestine will be sewn or stapled back together. This procedure is called an
anastomosis
.
Anastomosis
An anastomosis is a surgical connection between two structures. It usually means a connection that is created between tubular structures, such as bl...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Surgeons can also do this surgery using a laparoscope. The laparoscope is an instrument that looks like a small telescope with a light and a video camera. It is inserted into your belly through a small cut. Video from the camera appears on a monitor in the operating room. This allows the surgeon to view inside your belly during surgery.
In surgery using a laparoscope:
- Three to five small cuts are made in your belly. The camera and other small tools will be inserted through these cuts.
- Your surgeon may also make a cut that is 2 to 3 inches (5 to 7.6 cm) long to put a hand through, if needed.
- Your belly will be filled with gas to allow the surgeon to see the area and perform the surgery with more room to work.
- The diverticulum is operated on as described above.
Why the Procedure Is Performed
Treatment is needed to prevent:
- Bleeding
-
Bowel obstruction
(a blockage in your intestine)
Bowel obstruction
Intestinal obstruction is a partial or complete blockage of the bowel. The contents of the intestine cannot pass through it.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Infection
- Inflammation
The most common symptom of Meckel diverticulum is painless bleeding from the rectum. Your stool may contain fresh blood or look black and tarry.
Risks
Risks for anesthesia and surgery in general are:
-
Allergic reactions to medicines or
breathing problems
Breathing problems
Breathing difficulty may involve:Difficult breathingUncomfortable breathingFeeling like you are not getting enough air
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Bleeding
,
blood clots
, or infection
Bleeding
Bleeding is the loss of blood. Bleeding may be:Inside the body (internally) Outside the body (externally)Bleeding may occur:Inside the body when blo...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleBlood clots
Blood clots are clumps that occur when blood hardens from a liquid to a solid. A blood clot that forms inside one of your veins or arteries is calle...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Risks for this surgery are:
- Damage to nearby organs in the body.
- Wound infections or the wound breaks open after surgery.
- Bulging tissue through the surgical cut. This is called an incisional hernia.
- The edges of your intestines that are sewn or stapled together (anastomosis) may come open. This may cause life-threatening problems.
- The area where the intestines are sewn together can scar and create blockage of the intestine.
-
Blockage of the intestine may occur later from
adhesions
caused by the surgery.
Adhesions
Adhesions are bands of scar-like tissue that form between two surfaces inside the body and cause them to stick together.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Before the Procedure
Tell your surgeon:
- If you are or could be pregnant
- What medicines you are taking, even medicines, supplements, or herbs you bought without a prescription
During the days before your surgery:
- You may be asked to stop taking drugs that make it hard for your blood to clot. Some of these are aspirin, ibuprofen (Advil, Motrin), vitamin E, warfarin (Coumadin), and clopidogrel (Plavix).
- Ask your doctor which drugs you should still take on the day of the surgery.
- If you smoke, try to stop. Ask your doctor or nurse for help quitting.
On the day of your surgery:
- Follow your doctor's instructions about when to stop eating and drinking.
- Take the medicines your doctor told you to take with a small sip of water.
- Arrive at the hospital on time.
After the Procedure
Most people stay in the hospital for 1 to 7 days depending on how extensive the surgery was. During this time, the doctors and nurses will carefully monitor you.
Treatment may include:
- Pain medicines
- Tube through your nose into your stomach to empty your stomach and relieve nausea and vomiting
You will also be given fluids and nutrition through a vein (IV) until your doctor or nurse feels you are ready to start drinking or eating. This could be as soon as the day after surgery.
You will need to follow up with your surgeon in a week or two after surgery.
Outlook (Prognosis)
Most people who have this surgery have a good outcome. But the results of any surgery depend on your overall health. Talk with your doctor about your expected outcome.
References
Harris JW, Evers BM. Small intestine. In: Townsend CM, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery: The Biological Basis of Modern Surgical Practice . 20th ed. Philadelphia, PA: Elsevier; 2017:chap 49.
Terhune KP, Tarpley JL. The management of diverticulosis of the small bowel. In: Cameron JL, Cameron AM, eds. Current Surgical Therapy . 11th ed. Philadelphia, PA: Elsevier Saunders; 2014:128-132.
Review Date: 9/17/2016
Reviewed By: Debra G. Wechter, MD, FACS, general surgery practice specializing in breast cancer, Virginia Mason Medical Center, Seattle, WA. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.