Orbital pseudotumor
Idiopathic orbital inflammatory syndrome (IOIS)
Orbital pseudotumor is the swelling of tissue behind the eye in an area called the orbit. The orbit is the hollow space in the skull where the eye sits. The orbit protects the eyeball and the muscles and tissue that surround it. Orbital pseudotumor does not spread to other tissues or places in the body.
Causes
The cause is unknown. It mostly affects young women, although it can occur at any age.
Symptoms
Symptoms may include:
- Pain in eye, and it may be severe
- Restricted eye movement
- Decreased vision
- Double vision
- Eye swelling (proptosis)
- Red eye (rare)
Exams and Tests
The health care provider will examine your eye. If you have signs of pseudotumor, additional tests will be done to make sure you don't have other conditions that may look like pseudotumor. The two most common other conditions are:
- A cancer tumor
- Thyroid eye disease
Tests may include:
- CT scan of the head
- MRI of the head
-
Ultrasound
of the head
Ultrasound
Ultrasound uses high-frequency sound waves to make images of organs and structures inside the body.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Skull x-ray
Skull x-ray
A skull x-ray is a picture of the bones surrounding the brain, including the facial bones, the nose, and the sinuses.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Biopsy
Biopsy
A biopsy is the removal of a small piece of tissue for laboratory examination.
Read Article Now Book Mark Article
Treatment
Mild cases may go away without treatment. More severe cases most often respond well to corticosteroid treatment. If the condition is very bad, the swelling may put pressure on the eyeball and damage it. Surgery may be needed to remove part of the bones of the orbit to relieve the pressure.
Outlook (Prognosis)
Most cases are mild and outcomes are good. Severe cases may not respond well to treatment and there may be some loss of vision. Orbital pseudotumor most often involves only one eye.
Possible Complications
Severe cases of orbital pseudotumor may push the eye forward so much that the lids cannot cover and protect the cornea. This causes the eye to dry out. The cornea may become cloudy or develop an ulcer. Also, the eye muscles may not be able to properly aim the eye which can cause double vision.
When to Contact a Medical Professional
People with this condition need regular follow up care with an eye doctor who is familiar with the treatment of orbital disease.
Call your provider right away if you have any of the following problems:
- Irritation of the cornea
- Redness
- Pain
- Decreased vision
References
Goodlick TA, Kay MD, Glaser JS, Tse DT, Chang WJ. Orbital disease and neuro-ophthalmology. In: Tasman W, Jaeger EA, eds. Duane's Ophthalmology . 2013 ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2013:vol 2, chap 14.
Karesh JW, On AV, Hirschbein MJ. Noninfectious orbital inflammatory disease. In: Tasman W, Jaeger EA, eds. Duane's Ophthalmology . 2013 ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2013:vol 2, chap 35.
Yanoff M, Cameron JD. Diseases of the visual system. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine . 25th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 423.
-
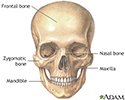
Skull anatomy - illustration
The skull is anterior to the spinal column and is the bony structure that encases the brain. Its purpose is to protect the brain and allow attachments for the facial muscles. The two regions of the skull are the cranial and facial region. The cranial portion is the part of the skull that directly houses the brain and the facial portion includes the rest of the bones of the skull.
Skull anatomy
illustration
-
Skull anatomy - illustration
The skull is anterior to the spinal column and is the bony structure that encases the brain. Its purpose is to protect the brain and allow attachments for the facial muscles. The two regions of the skull are the cranial and facial region. The cranial portion is the part of the skull that directly houses the brain and the facial portion includes the rest of the bones of the skull.
Skull anatomy
illustration
Review Date: 8/20/2016
Reviewed By: Franklin W. Lusby, MD, ophthalmologist, Lusby Vision Institute, La Jolla, CA. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.