Throat or larynx cancer
Vocal cord cancer; Throat cancer; Laryngeal cancer; Cancer of the glottis; Cancer of oropharynx or hypopharynx
Throat cancer is cancer of the vocal cords, larynx (voice box), or other areas of the throat.
Causes
People who smoke or use tobacco are at risk of developing throat cancer. Drinking too much alcohol over a long time also increases risk. Smoking and drinking alcohol combined lead to an increased risk for throat cancer.
Most throat cancers develop in adults older than 50. Men are more likely than women to develop throat cancer.
Symptoms
Symptoms of throat cancer include any of the following:
- Abnormal (high-pitched) breathing sounds
- Cough
- Coughing up blood
- Difficulty swallowing
- Hoarseness that does not get better in 3 to 4 weeks
- Neck or ear pain
- Sore throat that does not get better in 2 to 3 weeks, even with antibiotics
- Swelling or lumps in the neck
- Weight loss not due to dieting
Exams and Tests
The health care provider will perform a physical exam. This may show a lump on the outside of the neck.
The provider may look in your throat or nose using a flexible tube with a small camera at the end.
Other tests that may be ordered include:
-
Biopsy
of suspected tumor
Biopsy
An oropharynx lesion biopsy is surgery in which tissue from an abnormal growth or mouth sore is removed and checked for problems.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Chest x-ray
-
CT scan of chest
CT scan of chest
A chest CT (computed tomography) scan is an imaging method that uses x-rays to create cross-sectional pictures of the chest and upper abdomen....
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
CT scan of head and neck
CT scan of head and neck
A head computed tomography (CT) scan uses many x-rays to create pictures of the head, including the skull, brain, eye sockets, and sinuses.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
MRI of the head or neck
MRI of the head or neck
A head MRI (magnetic resonance imaging) is an imaging test that uses powerful magnets and radio waves to create pictures of the brain and surrounding...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
PET scan
PET scan
A positron emission tomography scan is a type of imaging test. It uses a radioactive substance called a tracer to look for disease in the body. A po...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Treatment
The goal of treatment is to completely remove the cancer and prevent it from spreading to other parts of the body.
When the tumor is small, either surgery or radiation therapy alone can be used to remove the tumor.
Radiation therapy
Radiation therapy uses high-powered x-rays, particles, or radioactive seeds to kill cancer cells.

When the tumor is larger or has spread to lymph nodes in the neck, a combination of radiation and chemotherapy is often used to save the voice box (vocal cords). If this is not possible, the voice box is removed. This surgery is called laryngectomy .
Chemotherapy
The term chemotherapy is used to describe cancer-killing drugs. Chemotherapy may be used to:Cure the cancerShrink the cancerPrevent the cancer from ...

Laryngectomy
Laryngectomy is surgery to remove all or part of the larynx (voice box) in your throat.
Support Groups
You can ease the stress of illness by joining a cancer support group . Sharing with others who have common experiences and problems can help you not feel alone.
Cancer support group
The following organizations are good resources for information on cancer:American Cancer Society -- www. cancer. orgCancerCare -- www. cancercare. or...
Outlook (Prognosis)
Throat cancers may be cured when detected early. If the cancer has spread ( metastasized ) to surrounding tissues or lymph nodes in the neck, about half of patients can be cured. If the cancer has spread to parts of the body outside the head and neck, the cancer is not curable. Treatment is aimed at prolonging and improving quality of life.
Metastasized
Metastasis is the movement or spreading of cancer cells from one organ or tissue to another. Cancer cells usually spread through the blood or the ly...

After treatment, therapy is needed to help with speech and swallowing. If the person is not able to swallow, a feeding tube will be needed.
Possible Complications
Complications of this type of cancer may include:
-
Airway obstruction
Airway obstruction
Breathing difficulty may involve:Difficult breathingUncomfortable breathingFeeling like you are not getting enough air
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Difficulty swallowing
- Disfigurement of the neck or face
- Hardening of the skin of the neck
-
Loss of voice
and speaking ability
Loss of voice
Hoarseness refers to a difficulty making sounds when trying to speak. Vocal sounds may be weak, breathy, scratchy, or husky, and the pitch or qualit...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Spread of the cancer to other body areas (metastasis)
When to Contact a Medical Professional
Call your provider if:
- You have symptoms of throat cancer, especially hoarseness or a change in voice with no obvious cause that lasts longer than 3 weeks
- You find a lump in your neck that does not go away in 3 weeks
Prevention
Do not smoke or use other tobacco. Limit or avoid alcohol use.
References
Armstrong WB, Vokes DE, Verma SP. Malignant tumors of the larynx. In: Flint PW, Haughey BH, Lund V, et al, eds. Cummings Otolaryngology: Head & Neck Surgery . 6th ed. Philadelphia, PA: Elsevier Saunders; 2015:chap 106.
National Cancer Institute. PDQ laryngeal cancer treatment. Bethesda, MD: National Cancer Institute. Date last modified: July 23, 2014. Available at: www.cancer.gov/cancertopics/pdq/treatment/laryngeal/HealthProfessional . Accessed: January 4, 2016.
National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology (NCCN guidelines): Head and neck cancers. Version 1.2015. Available at: www.nccn.org/professionals/physician_gls/pdf/head-and-neck.pdf . Accessed: January 4, 2016.
-
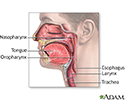
Throat anatomy - illustration
Structures of the throat include the esophagus, trachea, epiglottis and tonsils.
Throat anatomy
illustration
-
Oropharynx - illustration
Food passes from the mouth to the oropharynx (back of the throat) to the esophagus.
Oropharynx
illustration
Review Date: 10/30/2015
Reviewed By: Sumana Jothi, MD, specialist in laryngology, Clinical Instructor UCSF Otolaryngology, NCHCS VA, SFVA, San Francisco, CA. Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.