Olivopontocerebellar atrophy
OPCA; Olivopontocerebellar degeneration; Multiple system atrophy cerebellar predominance; MSA-C
Olivopontocerebellar atrophy (OPCA) is a disease that causes areas deep in the brain, just above the spinal cord, to shrink (atrophy).
Causes
OPCA can be passed down through families (inherited form). It can also affect people without a known family history (sporadic form).
Researchers have identified certain genes that are involved in the inherited form of this condition.
The cause of OPCA in people with the sporadic form is not known. The disease slowly gets worse (is progressive).
OPCA is slightly more common in men than in women. The average age of onset is 54 years old.
Symptoms
Symptoms tend to start at a younger age in people with the inherited form. The main symptom is clumsiness ( ataxia ) that slowly gets worse. There may also be problems with balance, slurring of speech, and difficulty walking.
Ataxia
Uncoordinated movement is due to a muscle control problem that causes an inability to coordinate movements. It leads to a jerky, unsteady, to-and-fr...

Other symptoms may include:
- Abnormal eye movements
- Abnormal movements
- Bowel or bladder problems
- Difficulty swallowing
- Lightheadedness when standing
- Muscle stiffness or rigidity, spasms, tremor
- Nerve damage (neuropathy)
-
Problems speaking due to
spasms of the vocal cords
Spasms of the vocal cords
Spasmodic dysphonia is difficulty speaking due to spasms (dystonia) of the muscles that control the vocal cords.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Sexual function problems
Exams and Tests
A thorough medical and nervous system examination, as well as a symptom and family history are needed to make the diagnosis.
There are genetic tests to look for the causes of some forms of the disorder. But, no specific test is available in many cases. An MRI of the brain may show changes in the size of affected brain structures, especially as the disease gets worse. But it is possible to have the disorder and have a normal MRI.
MRI of the brain
A head MRI (magnetic resonance imaging) is an imaging test that uses powerful magnets and radio waves to create pictures of the brain and surrounding...

Other tests may be done to rule out other conditions. These may include swallowing studies to see if a person can safely swallow food and liquid.
Treatment
There is no specific treatment or cure for OPCA. The aim is to treat the symptoms and prevent complications. This may include:
- Tremor medicines, such as those for Parkinson disease
- Speech and physical therapy
- Ways to prevent choking
- Walking aids to help with balance and prevent falls
Outlook (Prognosis)
OPCA slowly gets worse, and there is no cure. The outlook is generally poor. But, it may be years before someone is very disabled.
Possible Complications
Complications of OPCA include:
- Choking
-
Infection from inhaling food into the lungs (
aspiration pneumonia
)
Aspiration pneumonia
Pneumonia is a breathing condition in which there is swelling or an infection of the lungs or large airways. Aspiration pneumonia occurs when food, ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Injury from falls
- Nutrition problems due to difficulty swallowing
When to Contact a Medical Professional
Call your health care provider if you have any symptoms of OPCA. You will need to be seen by a neurologist. This person is a doctor who treats nervous system problems.
References
Jankovic J, Lang AE. Diagnosis and assessment of Parkinson disease and other movement disorders. In: Daroff RB, Jankovic J, Mazziotta JC, Pomeroy SL, eds. Bradley's Neurology in Clinical Practice . 7th ed. Philadelphia, PA: Elsevier; 2016:chap 23.
-
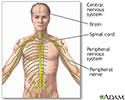
Central nervous system - illustration
The central nervous system is comprised of the brain and spinal cord. The peripheral nervous system includes all peripheral nerves.
Central nervous system
illustration
Review Date: 5/30/2016
Reviewed By: Amit M. Shelat, DO, FACP, Attending Neurologist and Assistant Professor of Clinical Neurology, SUNY Stony Brook, School of Medicine, Stony Brook, NY. Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.