Restless legs syndrome and related disorders
Willis-Ekbom disease; Ekbom's syndrome
An in-depth report on the causes, diagnosis, treatment, and prevention of RLS.
Highlights
Overview
- Restless legs syndrome (RLS) is a condition in which one has feelings of "pulling, searing, drawing, tingling, bubbling, or crawling" beneath the skin, usually in the calf area. This causes an irresistible urge to move the legs. The sensations can also affect the thighs, feet, and sometimes, even the arms.
- It can be a temporary problem (such as during pregnancy or while taking antidepressant medication) or a chronic, long-term issue. It can develop from several medical conditions and genetic risk factors.
RLS and PLMD
- Periodic limb movement disorder (PLMD) often accompanies RLS. It is a condition where leg muscles contract and jerk every 20 to 40 seconds during sleep. These movements may last less than 1 second, or as long as 10 seconds.
- Unlike RLS, contractions in PLMD usually do not wake patients, although bed partners may be wakened by the movements.
- Four out of five people who have RLS also report having PLMD, but only about a third of people with PLMD also have RLS.
Treatment
- Treatment often includes over-the-counter remedies, lifestyle changes, or iron supplements, particularly in cases where a lack of iron has been identified. Prescription medications can provide good relief of frequent or severe symptoms.
- Drugs to treat RLS include dopaminergic agonists, hypnotics, opioids, nonopioids, antiepileptic drugs, antidepressants, and others. Only a few drugs are FDA approved to treat RLS (ropinirole, pramipexole, rotigotine, gabapentin enacarbil). The rest are used off-label. Medicine is carefully chosen based on the intensity and duration of symptoms.
- Long-term treatment with dopaminergic agonists, can lead to tolerance (reduced response over time) and augmentation (worsening of symptoms with ongoing treatment).
Criteria and Guidelines
- The International Restless Legs Syndrome Study Group (IRLSSG) have updated and simplified diagnostic criteria for pediatric RLS. The criteria stress the understanding of specific words used by children in describing pain.
- The American Academy of Sleep Medicine issued updated guidelines in 2012 for the treatment of restless legs syndrome and periodic limb movement disorder in adults.
Introduction
Restless legs syndrome (RLS) is a poorly understood movement disorder that affects 3 to 15% of the general population. The problem can occur in both children and adults. Although effective treatments are available, RLS often goes undiagnosed.
Symptoms of RLS. The core symptom of RLS is an irresistible urge to move the legs. Some people describe this symptom as a sense of unease and weariness in the lower leg. The sensations are aggravated by rest and relieved by movement. Specific characteristics of RLS include:
- Uncomfortable feelings of "pulling, searing, drawing, tingling, bubbling, or crawling" beneath the skin, usually in the calf area, causing an irresistible urge to move the legs. These sensations occur mostly in the lower legs, but they can sometimes affect the thighs, feet, and even in the arms. These may be the first symptoms of RLS in some people.
- Semi-rhythmic movements during sleep known as periodic limb movement disorder (PLMD), which occurs in about 4 out of 5 patients with RLS. See description below.
- Itching and pain, particularly aching pain.
- Symptoms usually occur at night when patients are most relaxed, with their legs at rest, lying down. In more severe cases, symptoms also occur during the day while sitting. Movement relieves the symptoms.
- RLS episodes between 10 p.m. and 4 a.m. Symptoms are often worse shortly after midnight and disappear by morning. If the condition becomes more severe, people may begin to have symptoms during the day, but the problem is always worse at night.
- Disruption of nighttime sleep due to the unpleasant sensations and uncontrollable urge to move the legs. Ignoring the urge to move the legs usually leads to tension build up until the legs jerk uncontrollably. Individuals who experience daytime symptoms may find it difficult to sit during air or car travel, or through classes or meetings.
Late-onset and Early-onset forms
Restless Legs Syndrome can be either an early-onset or late-onset form of the syndrome. Each form may have different characteristics:
- People with early-onset RLS (occurring in the teenage years or earlier) tend to have a family history of the disorder. They usually have RLS without accompanying pain.
- People with late-onset RLS usually do not have a family history of RLS. The condition is more likely to result from a problem with the nervous system. Symptoms may also include pain in the lower legs.
Periodic Limb Movement Disorder
Periodic limb movement disorder (PLMD) is also known as nocturnal myoclonus. Characteristics of PLMD include:
- Nighttime episodes that usually peak near midnight (similar to the pattern in RLS).
- Contractions and jerking of the leg muscles every 20 to 40 seconds during sleep. These movements may last less than 1 second, or as long as 10 seconds.
- Movements of PLMD that do not wake the person who actually has it, but they are often noticed by their bed partner. This condition is distinct from the brief and sudden movements that occur just as people are falling asleep, which can interrupt sleep.
- Association with RLS: Four out of five people who have RLS also report having PLMD, but only a third of people with PLMD report having RLS.
While treatments for the two conditions are similar, PLMD is a separate syndrome. PLMD is also very common in narcolepsy, a sleep disorder that causes people to fall asleep suddenly and uncontrollably.
Causes
The main cause of RLS is unknown. Scientists are researching nervous system problems that may arise in either the spinal cord or the brain. One theory suggests that low levels of the brain chemical dopamine causes RLS.
RLS may often have a genetic basis, particularly in those who develop it before age 40. RLS in older adults is less likely to be inherited.
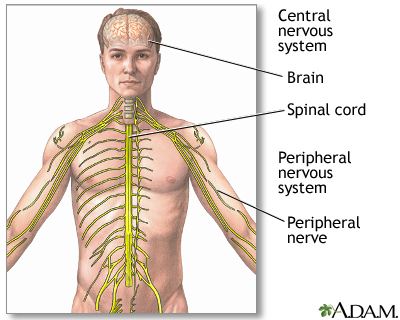
The central nervous system includes the brain and spinal cord. The peripheral nervous system includes all peripheral nerves.
Genetic Factors
People with RLS often have a family history of the disorder. There are at least six genetic factors that may play a part. Two of the genes are linked to spinal cord development. However, more research is needed to show a link between these genetic factors and dopamine or iron-regulating systems.
Neurological Abnormalities
Dopamine and Neurologic Abnormalities in the BrainSeveral studies support the theory that an imbalance in neurotransmitters (chemical messengers in the brain), notably dopamine, may play a part in RLS. Dopamine triggers numerous nerve impulses that affect muscle movement. The effect is similar to that seen in Parkinson disease. In addition, drugs that increase dopamine levels treat both disorders. However, Parkinson disease itself does not seem to increase the risk for RLS and RLS early in life does not increase the risk of Parkinson later on.
Neurologic Abnormalities in the SpineOther research suggests that RLS may be due to nerve impairment in the spinal cord. Researchers had thought that such abnormalities began in nerve pathways in the lower spine. However, some patients with RLS have symptoms in the arms, which indicates that the upper spine may also be involved.
NeuropathySome experts suggest that RLS, particularly if it occurs in older adults, may be a form of neuropathy, which is an abnormality in the nervous system outside the spine and brain. So far, there is no evidence to support a cause and effect relationship between neuropathy and RLS.
Abnormalities of Iron Metabolism
Iron deficiency, even at a level too mild to cause anemia, has been linked to RLS in some people. Some research suggests that RLS in some people may be due to a problem with getting iron into cells that regulate dopamine in the brain. Some studies have reported RLS in a quarter to a third of people with low iron levels.
Deficiencies in Cortisol
Other research suggests that low levels of the hormone cortisol in the evening and early night hours may be related to RLS. Low-dose cortisol injections have reduced symptoms in some people.
Causes of Periodic Limb Movement DisorderThe causes of PLMD are not clear. Some research suggests that it may be due to abnormalities in the autonomic nervous system, which regulates the involuntary actions of the smooth muscles, heart, and glands.
Risk Factors
RLS may affect 1.5 to 2.7% of the general population. Some studies have shown that it may be much more common. It is more common in women than in men, and in North America and Europe, its frequency increases with age.
Family History
As many as two-thirds of people with RLS have a family history of the disorder, and are more likely to develop RLS before they turn 40. People who develop the condition at a later age are less likely to have a family history of RLS. RLS is also more common in people from northern and western Europe, adding support for the theory that some cases have a genetic basis.
Attention Deficit Hyperactivity Disorder
Up to a quarter of children diagnosed with attention-deficit hyperactivity disorder (ADHD) may also have RLS, sleep apnea, and PLMD. These conditions may actually contribute to inattentiveness and hyperactivity. The disorders have much in common, including poor sleep habits, twitching, and the need to get up suddenly and walk about frequently. Some evidence suggests that the link between the diseases may be a deficiency in the brain chemical dopamine.
Pregnancy
About 1 in 5 pregnant women report having RLS. The condition usually goes away within a month of delivery. RLS in pregnancy has been linked to deficiencies in iron and the B vitamin folate.
Dialysis
RLS is relatively common in people undergoing kidney dialysis. Up to two-thirds of patients report this problem. Symptoms often disappear after a kidney transplant.
Anxiety Disorders
Anxiety can cause restlessness and agitation at night. These symptoms can cause RLS or strongly resemble the condition.
Other Conditions Associated with Restless Legs Syndrome
The following medical conditions are also associated with RLS, although the relationships are not clear. In some cases, these conditions may contribute to RLS. Others may have a common cause, or they may coexist due to other risk factors:
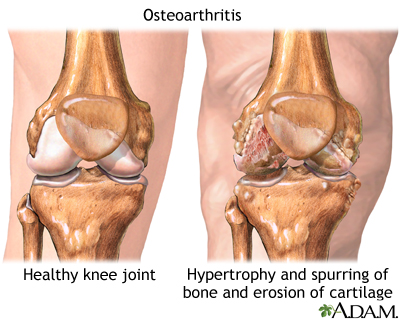
- Osteoarthritis (degenerative joint disease). About three-quarters of patients with RLS also have osteoarthritis, a common condition affecting older adults.
- Varicose veins. Varicose veins occur in about 1 in 7 patients with RLS.
- Obesity
- Diabetes. People with type 2 diabetes may have higher rates of secondary RLS. Nerve pain (neuropathy) related to their diabetes cannot fully explain the higher rate of RLS.
- Hypertension (high blood pressure)
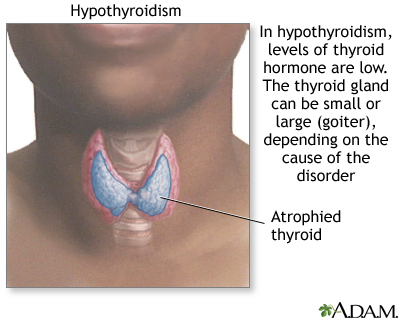
- Hypothyroidism. In this condition, the thyroid gland does not make enough hormones.
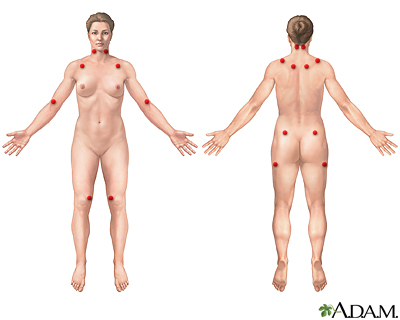
- Fibromyalgia. A chronic pain of unknown cause.
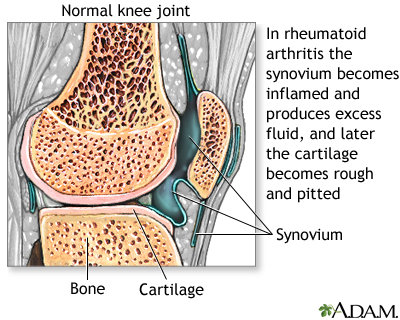
- Rheumatoid arthritis
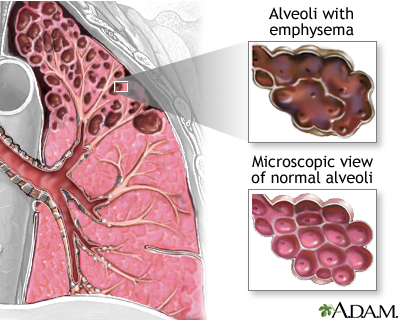
- Emphysema. This lung disease is often caused by smoking.
- Chronic alcoholism
- Sleep apnea (pauses in breathing during sleep) and snoring
- Chronic headaches
- Brain or spinal injuries
- Many muscle and nerve disorders. Of particular interest is hereditary ataxia, a group of genetic diseases that affects the central nervous system and causes loss of motor control. Researchers believe that hereditary ataxia may supply clues to the genetic causes of RLS.
- Attention-deficit hyperactivity disorder (ADHD) in children
- Psychiatric disorders, such as depression.
Osteoarthritis is a chronic disease of the joint cartilage and bone, once thought to result from "wear and tear" on a joint, although there are other causes such as trauma, and metabolic disorders. Joints appear swollen, are stiff and painful, and usually feel worse the more they are used throughout the day.
Environmental and Dietary Factors
The following environmental and dietary factors can trigger or worsen RLS:
- Iron deficiency. People who are deficient in iron are at risk for RLS, even if they do not have anemia
- Folic acid or magnesium deficiencies
- Smoking
- Alcohol abuse
- Caffeine. Coffee drinking is specifically associated with PLMD.
- Stress
- Fatigue
- Prolonged exposure to cold
Medications
Drugs that may worsen or provoke RLS include:
- Antidepressants
- Antipsychotic drugs
- Anti-nausea drugs
- Calcium channel blockers (mostly used to treat high blood pressure)
- Metoclopramide (used to treat various digestive diseases)
- Antihistamines
- Oral decongestants
- Diuretics
- Asthma drugs
- Spinal anesthesia (anesthesia-induced RLS typically disappears on its own within several months)
Risk Factors for Periodic Limb Movement Disorder
About 6% of the general population has PLMD. However, the prevalence in older adults is much higher, reaching almost 60%. Studies suggest that PLMD may be especially common in elderly women. As with RLS, there are many conditions that are associated with PLMD. They include sleep apnea, spinal cord injuries, stroke, narcolepsy, and diseases that destroy nerves or the brain over time. Certain drugs, including some antidepressants and anti-seizure medications, may also contribute to PLMD.
Complications
RLS rarely results in any serious consequences. However, recurring severe symptoms may cause considerable mental distress, loss of sleep, and daytime sleepiness. Because the condition is worse while resting, people with severe RLS may avoid activities that involve extended periods of sitting, such as attending movies or traveling long distances.
Sleep Deprivation
Inability to sleep during the night due to RLS symptoms and subsequent daytime sleepiness can cause mood changes. Lack of sleep can also contribute to workplace errors and car crashes.
Effect on Daily Performance and ActivitiesSleeplessness has a negative effect on the ability to function while awake. Areas that can be affected include:
- Concentration. Loss of deep sleep can impair the brain's ability to process information.
- Task performance. Missing several hours of sleep every night can negatively affect a person's mood and ability to function. People deprived of sleep show lowered performance levels on a par with those of people who are intoxicated.
- Learning. The extent to which sleeplessness impairs learning is unclear. Some studies have reported problems in memorization.
Psychiatric Effects
People with RLS are more apt to suffer problems such as social isolation, frequent daytime headaches, and depression. They may also complain of lower sex drive and other problems related to insufficient sleep.
RLS can contribute to insomnia. Insomnia itself can increase the activity of hormones and pathways in the brain that produce emotional problems. Even modest changes in waking and sleeping patterns can have significant effects on a person's mood. In some cases, ongoing insomnia may even predict mood disorders in the future.
It is not clear if RLS is responsible for mood problems or if anxiety or depression contributes to RLS. Anxiety can cause agitation and leg restlessness that resemble RLS. Depression and RLS symptoms also overlap. Certain types of antidepressant drugs, such as serotonin reuptake inhibitors, can increase periodic limb movements during sleep. Medicines used to treat RLS can cause or increase existing psychiatric conditions. Dopamine agonists, for example, can increase compulsive behaviors, such as gambling.
Diagnosis
A diagnosis of RLS often relies mainly on the patient's description of symptoms. The first step in diagnosis is usually to gather information on a person's sleep and personal history. The doctor may ask the following questions:
- How would you describe your sleep problem?
- How long have you had this sleep problem? How long does it take you to fall asleep?
- How many times a week does the problem occur?
- How restful is your sleep?
- What do your leg problems feel like (such as cramps, twitching, and crawling feelings)?
- What is your sleep environment like? Noisy? Not dark enough?
- What medications are you taking (including the use of antidepressants and self-medications -- such as herbs, alcohol, and over-the-counter or prescription drugs)?
- Are you taking or withdrawing from stimulants, such as coffee or tobacco? How much alcohol do you drink per day?
- What stresses or emotional factors may be present in your life? Have you experienced any significant life changes?
- Do you snore or gasp during sleep? (This may be an indication of sleep apnea. Sleep apnea is a condition in which breathing stops for short periods many times during the night. It may worsen symptoms of RLS or insomnia.)
- If you have a bed partner, does he or she notice that you have jerking legs, interrupted breathing, or thrashing while you sleep?
- Are you a shift worker?
- Do you have a family history of RLS or PLMD, "growing pains" at night, or night walking?
To help answer these questions, the patient may need to keep a sleep diary for 2 weeks. The patient should record all sleep-related information, including responses to the questions listed above on a daily basis. Using an extended-play audio or videotape to record sleep behavior can be very helpful in diagnosing sleep apnea. A bed partner can help provide information based on observations of the patient's sleep behavior.
The International Restless Legs Syndrome Study Group (IRLSSG) have updated and simplified diagnostic criteria for pediatric RLS. The criteria stress the understanding of specific words used by children in describing pain.
Sleep Disorders Centers
Some patients may need to consult a sleep specialist or go to a sleep disorders center in order for the problem to be diagnosed. At most centers, patients undergo in-depth testing supervised by a team of consultants from various specialties, who can provide both physical and psychiatric evaluations. Centers should be accredited by the American Academy of Sleep Medicine.
Signs that may indicate the need to go to a sleep disorders center are:
- Insomnia due to psychological disorders
- Sleeping problems due to substance abuse
- Snoring and sudden awakening with gasping for breath (possible sleep apnea)
- Severe RLS
- Persistent daytime sleepiness
- Sudden episodes of falling asleep during the day (possible narcolepsy)
Polysomnography
Overnight polysomnography involves a series of tests to measure different functions during sleep. This type of evaluation is typically performed in a sleep center. It can help rule out sleep apnea when this problem is suspected or evaluate the effectiveness of RLS treatments.
To undergo the test, the patient arrives about 2 hours before bedtime without having made any changes in daily habits. This test electronically monitors the patient through the various sleep stages. Polysomnography tracks the following:
- Brain waves
- Body movements
- Breathing
- Heart rate
- Eye movements
- Changes in breathing and blood levels of oxygen
Actigraphy
Actigraphy uses a small wristwatch-like device (such as Actiwatch) worn on the wrist or ankle. The device monitors the sleep quality in people suspected of having RLS, PLMD, insomnia, sleep apnea, and other sleep-related conditions. It measures and records muscle movements during sleep. For example, with PLMD, actigraphy can provide information on how long movements last and the number of times they occur. It can also track whether PLMD occurs in both legs at the same time, and the effect it has on sleep. Actigraphy is not as accurate as polysomnography because it cannot measure all the biological effects of sleep. It is more accurate than a sleep log, however, and very helpful for recording long periods of sleep.
Sleepiness Scale
The Epworth sleepiness scale uses a simple questionnaire to measure excessive sleepiness during eight situations.
The Epworth Sleepiness Scale |
||
Situation |
Chance of Dosing |
|
|
Sitting and reading |
(Indicate a score of 0 to 3) 0 = no chance of dozing 1= slight chance of dozing 2 = moderate chance of dozing 3 = high chance of dozing |
|
|
Watching TV |
(Indicate a score of 0 to 3)
0 = no chance of dozing 1= slight chance of dozing 2 = moderate chance of dozing 3 = high chance of dozing |
|
|
Sitting inactive in a public place |
(Indicate a score of 0 to 3)
0 = no chance of dozing 1= slight chance of dozing 2 = moderate chance of dozing 3 = high chance of dozing |
|
|
Riding as a passenger in a car for an hour without a break |
(Indicate a score of 0 to 3)
0 = no chance of dozing 1= slight chance of dozing 2 = moderate chance of dozing 3 = high chance of dozing |
|
|
Lying down to rest in the afternoon when circumstances permit |
(Indicate a score of 0 to 3)
0 = no chance of dozing 1= slight chance of dozing 2 = moderate chance of dozing 3 = high chance of dozing |
|
|
Sitting and talking to someone |
(Indicate a score of 0 to 3)
0 = no chance of dozing 1= slight chance of dozing 2 = moderate chance of dozing 3 = high chance of dozing |
|
|
Sitting quietly after a lunch without alcohol |
(Indicate a score of 0 to 3)
0 = no chance of dozing 1= slight chance of dozing 2 = moderate chance of dozing 3 = high chance of dozing |
|
|
Sitting in a car while stopped for a few minutes in traffic |
(Indicate a score of 0 to 3)
0 = no chance of dozing 1= slight chance of dozing 2 = moderate chance of dozing 3 = high chance of dozing |
|
Score Results1 to 6: Getting enough sleep. 4 to 8: Tends to be sleepy but is average. 9 and over: Very sleepy and suggestive of sleep-disordered breathing. Patient should seek medical advice. |
||
Diagnosing Iron Deficiency Anemia and Its Causes
Because of the high association between RLS and iron deficiency, a test for low iron stores should be part of the diagnostic workup in RLS. There are two steps in making this diagnosis:
- The first step is to determine if a person is actually deficient in iron.
- If iron stores are low, the second step is to diagnose the cause of the iron deficiency, which will help determine treatment.
The following can help determine if a person is iron deficient:
- Blood cells viewed under the microscope appear pale (hypochromic) and abnormally small (microcytic). These observations suggest iron deficiency, as well as anemia resulting from chronic disease and thalassemia (an inherited blood disorder).
- Low levels of hemoglobin and iron further suggest iron deficiency, but can also occur in cases of anemia due to chronic disease. Low levels of ferritin, a protein that binds to iron typically indicate a lack of iron in the body. However, normal levels of ferritin in the blood do not always mean a patient has enough iron. For example, pregnant women in their third trimester or patients with a chronic disease may not have enough iron even with normal or high ferritin levels.
-
A test that measures a factor called serum transferrin receptor (sTfR) helps in identifying iron deficiency in some patients, including the elderly with chronic diseases and possibly pregnant women. When iron deficiency anemia is diagnosed, the next step is to determine the cause of the iron deficiency itself. Menstrual blood loss is a common cause of iron deficiency in women of reproductive age. Tests to check for an underlying cause of iron deficiency, such as gastrointestinal (digestive tract) bleeding, are particularly important in men, postmenopausal women, and children.
Anemia
An in-depth report on the types, diagnosis, treatment, and prevention of anemia.
 Image
ImageRead Article Now Book Mark Article
Other Laboratory Tests
The following laboratory tests may be helpful in determining causes of RLS or identifying conditions that rule it out.
- Blood glucose tests for diabetes
- Tests for kidney problems
- In certain cases, tests for thyroid hormone, magnesium, and folate levels
- Electromyography (recording the electrical activity of muscles) for neuropathy, radiculopathy (problem with the nerve roots), myelopathy (problem with the spinal cord)
- Central nervous system MRI for myelopathy or stroke
Ruling Out Other Leg Disorders
In addition to other sleep-related leg disorders, many other medical conditions may have features that resemble RLS. The doctor will need to consider these disorders in making a diagnosis.
Peripheral NeuropathiesPeripheral neuropathies are nerve disorders in the hands or feet, which can produce pain, burning, tingling, or shooting sensations in the arms and legs. Several conditions can cause these disorders; diabetes is a very common cause of painful peripheral neuropathies. Other causes include alcoholism, chemotherapy, rheumatoid arthritis, systemic lupus erythematosus, amyloidosis, HIV infection, kidney failure, and certain vitamin deficiencies. Symptoms of peripheral neuropathies may mimic RLS. However, unlike RLS, these disorders are not usually associated with restlessness. Also, movement does not relieve the discomfort, and the problem does not worsen at bedtime.
AkathisiaAkathisia is a state of restlessness or agitation, and feelings of muscle quivering. A condition called hypotensive akathisia is caused by failure in the autonomic nervous system. Unlike RLS, it occurs at any time of the day, and only when the patient is sitting -- not lying down. Drugs that are used to treat nausea, schizophrenia and other psychoses can cause akathisia. The condition also occurs when drugs to treat Parkinson disease are stopped.
Painful Legs and Moving Toes SyndromeThis is a rare disorder that affects one or both legs. Painful legs and moving toes syndrome is marked by a constant, deep, throbbing ache in the limbs and involuntary toe movements. The discomfort may be mild or severe. The problem gets worse with activity and usually stops during sleep. Most of the time, the cause is unknown, although it may arise from spinal injuries or herpes zoster infection. The condition is difficult to treat, but the drug baclofen, combined with either clonazepam or carbamazepine, has shown some success. Other treatments that may help include orthotic shoe inserts and therapy using transcutaneous electrical nerve stimulation (TENS).
Meralgia ParestheticaAn uncommon nerve condition, meralgia paresthetica causes numbness, pain, tingling, or burning on the front and side of the thigh. It usually occurs on one side of the body. The condition may be caused by compression of the thigh nerve as it passes through the pelvis. The problem typically occurs in those with diabetes, obesity or both, and can affect people of all ages. It often goes away on its own.
Nocturnal (Nighttime) Leg Cramps
Cramps that awaken people during sleep are very common, but they are not RLC or PLMD. Nocturnal leg cramps can be very painful and may cause the person to jump out of bed in the middle of the night. They typically affect a specific area of the calf or the sole of the foot.
What Are Nocturnal Leg Cramps?
Benign nocturnal leg cramps (charley horse) are muscle spasms in the calf. They can occur one or many times during the night. Cramping may also occur in the soles of the feet. Typically, cramps last from a few seconds to a few minutes. Some people experience them regularly, others rarely.
Causes of Nocturnal Leg CrampsIn most cases, the cause of nocturnal leg cramps remains unknown. Among the conditions that might cause leg cramps are:
- Calcium and phosphorus imbalances, particularly during pregnancy
- Disorders of the peripheral nerves, such as polyneuropathy due to diabetes, chemotherapy, kidney disease, or others
- Low potassium or sodium levels
- Overexertion, standing on hard surfaces for long periods, or prolonged sitting (especially with the legs contorted)
- Having structural disorders in the legs or feet (such as flat feet)
- Medical causes of muscle cramping which include hypothyroidism, Addison's disease, uremia, hypoglycemia, anemia, and certain medications. Various diseases that affect nerves and muscles, such as Parkinson disease, cause leg cramps.
Nocturnal leg cramps occur at all ages but peak at different times. They are particularly common in adolescence, during pregnancy, and in older age, affecting up to 70% of adults over age 50 at some point.
Pregnant women and those taking diuretics are also at risk for leg cramps because of low calcium levels and an imbalance in calcium and phosphorus.
Consequences of Nocturnal Leg Cramps. Nocturnal leg cramps rarely have serious consequences. However, they can be extremely painful and long lasting. Severe symptoms that occur often can cause chronic insomnia and considerable mental distress.Managing Nocturnal Leg Cramps
Ways to relieve a cramp once it has begun include:
- Straightening the leg, flexing the foot upward toward the knee, or grabbing the toes and pulling them toward the knee.
- Walking, or shaking the affected leg then elevating it.
If soreness persists, a warm bath or shower or an ice pack may bring relief.
Lifestyle Tips for Preventing Nocturnal Leg CrampsNighttime leg cramps are generally treated with lifestyle changes.
- Drink plenty of water (at least 6 to 8 glasses daily) to maintain adequate fluid levels. Nightly stretching exercises may help prevent leg cramps. (This are generally recommended for RLS, as well).
- Stretch leg muscles by standing about arm's length away from a wall. Keeping heels flat on the floor, lean forward and slowly move hands up the wall to achieve a comfortable stretch.
- Alternately, pedal for a few minutes on a stationary bicycle at bedtime.
- Place loose covers over the toes and feet while in bed. This prevents the toes and feet from pointing, which causes calf muscles to contract and cramp. Propping the feet up higher than the torso may also help.
- Swim regularly and do water exercises to help keep muscles stretched.
- Wear supportive footwear to help reduce leg cramps.
Quinine had been widely used to prevent leg cramping. The U.S. Food and Drug Administration (FDA) banned its sale over the counter because it reportedly caused some serious, although rare, side effects. These side effects include bleeding problems and heart irregularities. Other, less serious side effects include headaches, vision problems, and rashes.
The FDA has since banned the marketing of most quinine drugs, cautioning against the off-label (non-approved) use of the drug to treat nocturnal leg cramps. Only one form of the drug, Qualaquin, is approved for sale. It is used for the treatment of some types of malaria. Pregnant women and people with liver problems should avoid quinine in any form. The FDA has issued a warning of serious, potentially life-threatening side effects resulting from the use of Qualaquin for nocturnal leg cramps. These side effects include dangerously low blood platelet counts (platelets help the blood clot) and permanent kidney damage.
SupplementsSome small studies indicate that the mineral magnesium, taken as magnesium citrate or magnesium lactate, may provide some benefit to people with leg cramps, including pregnant women. Supplements tried for leg cramps include vitamin B complex, vitamin E, calcium, and potassium or sodium chloride, but these do not appear to be very effective. Other drugs that may help include diltiazem (a calcium channel blocker) and naftidrofuryl (unavailable in the United States).
Treatment
Treatment for complaints of sleeplessness and RLS focus on improving sleep and eliminating possible causes of RLS. Initially, doctors normally try to achieve these goals without the use of drugs. A non-drug approach is a particularly important first step for elderly patients.
- The doctor should first try to treat any underlying medical conditions that may be causing restless legs.
- If medications may be causing RLS, the doctor should try to prescribe alternatives.
If the cause cannot be determined, measures to improve sleep habits and relaxation techniques are the best first steps. These approaches may help, even if medicines may be needed later on.
Lifestyle Changes
Some people report that making the following changes help control RLS:
- Taking hot baths or using cold compresses.
- Quitting smoking.
- Getting enough exercise during the day.
- Doing calf stretching exercises at bedtime.
- Using ergonomic measures. For example, working at a high stool where legs can dangle helps some people. Also, sitting in an aisle seat during meetings or airplane travel can allow for more leg movement.
- Changing sleep patterns. Some people report that symptoms do not occur when they sleep in the late morning. Therefore, patients may consider changing their sleep patterns if feasible.
- Avoiding caffeine, alcohol, and nicotine also improves some cases of RLS.
Some patients have tried alternative treatments for RLS, such as acupuncture and massage. To date, however, there is not enough data on the effectiveness of these treatments.
Dietary Iron
RLS is associated with iron deficiency, so people with the condition should make sure they get enough iron in their diet. [For more information, see In-Depth Report #57: Anemia .] Iron is found in foods either in the form of heme or non-heme iron:
Anemia
An in-depth report on the types, diagnosis, treatment, and prevention of anemia.

|
|
|
| Read Article Now | Book Mark Article |
- Foods containing heme iron are the best for increasing or maintaining healthy iron levels. Such foods include clams, oysters, organ meats, beef, pork, poultry, and fish.
- Non-heme iron is less well absorbed. Over half the iron in meat is non-heme. Eggs, dairy products, and iron-containing vegetables (including dried beans and peas) have only the non-heme form. Other sources of non-heme iron include iron-fortified cereals, bread, and pasta products, dark green leafy vegetables (such as chard, spinach, mustard greens, and kale), dried fruits, nuts, and seeds.
Iron Supplements
Iron supplements may reduce symptoms in people with RLS who are also iron deficient. Patients should use them only when dietary measures have failed. Iron supplements do not appear to be useful for RLS patients with normal or above normal iron levels.
Supplement FormsTo replace iron, the preferred forms of iron tablets are ferrous salts, usually ferrous sulfate (Feosol, Fer-In-Sol, Mol-Iron). Other forms include ferrous fumarate (Femiron, Ferro-Sequels, Feostat, Fumerin, Hemocyte, Ircon), ferrous gluconate (Fergon, Ferralet, Simron), polysaccharide-iron complex (Niferex, Nu-Iron), and carbonyl iron (Elemental Iron, Feosol Caplet, Ferra-Cap). Specific brands and forms may have certain advantages.
RegimenA reasonable approach for patients with RLS is to take 65 mg of iron (or 325 mg of ferrous sulfate) along with 100 mg of vitamin C on an empty stomach, 3 times a day.
IMPORTANT: As few as 3 adult iron tablets can poison, and even kill, children. This includes any form of iron pill. No one, not even adults, should take a double dose of iron if they miss one dose.Tips for taking iron are:
- For best absorption, take iron between meals. (Iron may cause stomach and intestinal disturbances. Some experts believe that you can take low doses of ferrous sulfate with food and avoid the side effects.)
- Always drink a full 8 ounces of fluid with an iron pill.
- Keep tablets in a cool place. Bathroom medicine cabinets may be too warm and humid, which may cause the pills to disintegrate.
Common side effects of iron supplements include the following:
- Constipation and diarrhea may occur but these side effects are rarely severe. However, iron tablets can aggravate existing digestive problems such as ulcers and ulcerative colitis.
- Nausea and vomiting may occur with high doses. You can control this by taking smaller amounts. Switching to ferrous gluconate may help some people with severe digestive problems.
- Black stools are normal when taking iron tablets. In fact, if stools do not turn black, the tablets may not be working effectively.
- Stools that appear tarry or have red streaks may indicate bleeding in the digestive tract, which may be causing iron deficiency. Other warning signs include cramps, sharp pains, or soreness in the stomach. Intestinal bleeding requires immediate medical attention.
- Acute iron poisoning is rare in adults, but can be fatal in children who take adult-strength tablets.
Iron tablets may also reduce the effectiveness of other drugs, including:
- Antibiotics. Tetracycline, penicillamine, and ciprofloxacin.
- Anti-Parkinson disease drugs. Methyldopa, levodopa, and carbidopa.
At least 2 hours should pass between doses of these drugs and doses of iron supplements.
[For additional information about iron supplements see In-Depth Report #57: Anemia .]
Anemia
An in-depth report on the types, diagnosis, treatment, and prevention of anemia.

|
|
|
| Read Article Now | Book Mark Article |
Exercise
Exercise early in the day helps achieve healthy sleep. Vigorous exercise too close to bedtime (1 to 2 hours before) may worsen RLS. A study found that people who walked briskly for 30 minutes, 4 times a week, improved minor sleep disturbances after 4 months. Regular, moderate exercise may help prevent RLS. However, patients report that either bursts of excessive energy or long sedentary periods can worsen symptoms.
Medications
The American Academy of Sleep Medicine recommends medications for RLS or PLMD only for persons who fit within strict diagnostic criteria, and who experience excessive daytime sleepiness as a result of these conditions. Excessive daytime sleepiness results from nighttime sleeplessness due to RLS or PLMD symptoms. Adverse effects are common and may be troublesome enough to prompt some patients to discontinue their RLS medications.
More research and physician training is needed to better diagnose and treat RLS with medications in children and adolescents. Little is known about the best way to treat RLS in general, but some experts suggest the following for adults:
- If lifestyle changes do not control the problem, over-the-counter pain relievers should be the first form of treatment.
- People with RLS should have a test for iron deficiency. If they are iron deficient, they should start treatment with iron supplements.
- Dopaminergic drugs (drugs that increase levels of dopamine) are the standard medicines for treating severe RLS, PLMD, or both.
- Other drugs may be helpful if dopaminergic drugs fail, or for patients who have frequent, but not nightly, symptoms. These include opiates (pain relievers), benzodiazepines (sedative hypnotic drugs), or anticonvulsants. However, benzodiazepines and opiates can become habit forming and addictive.
Tylenol and Non-Steroidal Anti-Inflammatory Drugs
Before taking stronger medications, people should try over-the-counter pain relievers, such as acetaminophen (Tylenol) or non-steroidal anti-inflammatory drugs (NSAIDs), which include ibuprofen (Advil, Motrin, Rufen), naproxen (Anaprox, Naprosyn, Aleve), and ketoprofen (Orudis KT, Actron).
Although NSAIDs work well, long-term use can cause stomach problems, such as ulcers, bleeding, and possible heart problems. The FDA has asked drug manufacturers of NSAIDs to include a warning label on their product that alerts users of an increased risk for heart-related problems and digestive tract bleeding.
Levodopa and Other Dopaminergic Drugs
Dopaminergic drugs increase the availability of the chemical messenger dopamine in the brain, and are the first-line treatment for severe RLS and PLMD. These drugs reduce the number of limb movements per hour, and improve the subjective quality of sleep. Patients with either condition who take these drugs have experienced up to 100% reduction in symptoms.
Dopaminergic drugs, however, can have severe side effects (they are ordinarily used for Parkinson disease). They do not appear to be as helpful for RLS related to dialysis as they do for RLS from other causes.
Dopaminergic drugs include dopamine precursors and dopamine receptor agonists.
Dopamine PrecursorsThe dopamine precursor levodopa (L-dopa) was once a popular drug for severe RLS, although today it is usually recommended only for patients with occasional symptoms who may take it nightly as needed. It may also be helpful for long car rides or plane trips. The standard preparations (Sinemet, Atamet) combine levodopa with carbidopa, which improves the action of levodopa and reduces some of its side effects, particularly nausea. Levodopa can also be combined with benserazide (Madopar) with similar results. Sinemet is commonly prescribed in America. Levodopa combinations are well tolerated and safe.
Levodopa acts fast, and the treatment is usually effective within the first few days of therapy.
Unfortunately, many studies report that patients suffer from augmentation (called augmentation) that occur earlier in the day in up to 70% of patients who take L-dopa. The risk is highest for patients who take daily doses, especially doses at high levels (greater than 200 mg/day). For this reason, patients should use L-dopa fewer than 3 times per week. The drug should be immediately discontinued if augmentation does occur. Following withdrawal from L-dopa, patients can switch to a dopamine receptor agonist.
A rebound effect (return of symptoms after the drug is discontinued) causes increased leg movements at night or in the morning as the dose wears off, or as tolerance to the drug builds up.
RegimensThe effects of L-dopa are apparent in 15 to 30 minutes. Dopamine receptor agonists, meanwhile, take at least 2 hours to start working. Some doctors recommend regular use of dopamine receptor agonists for patients who experience nightly symptoms, and L-dopa for those whose symptoms occur only occasionally.
Side EffectsCommon side effects of dopaminergic drugs vary but may include feeling faint or dizzy (especially when standing up), headaches, abnormal muscle movements, rapid heartbeat, insomnia, bloating, chest pain, and dry mouth. Nausea may be especially common. In rare cases, dopaminergic drugs can cause hallucinations or lung disease.
Because these drugs may cause daytime drowsiness, patients should be extremely careful while driving or performing tasks that require concentration.
Long-term use of dopaminergic drugs can lead to tolerance, in which the drugs become less effective.
Rebound effect, augmentation, and tolerance can reduce the value of dopaminergic drugs in the treatment of RLS. Using the lowest dose possible can minimize these effects.
Withdrawal SymptomsPatients who withdraw from these drugs typically experience severe RLS symptoms for the first 2 days after stopping. RLS eventually returns to pre-treatment levels after about a week. The longer a patient uses these drugs, the worse their withdrawal symptoms.
Withdrawal from dopamine precursors or dopamine agonists can lead to a serious, potentially life-threatening condition called Neuroleptic Malignant Syndrome. This disorder causes muscle stiffness and breakdown, fever, rigidity and confusion. One should never abruptly stop these medications with out first talking to their doctor.
Dopamine Receptor AgonistsDopamine receptor agonists (also called dopamine agonists) mimic the effects of dopamine by acting on dopamine receptors in the brain. They are now generally preferred to L-dopa (see below). Because they have fewer side effects than L-dopa, including rebound effect and augmentation, these drugs may be used on a daily basis. As the newer drugs are taken for longer periods and at higher doses, however, their augmentation rates may become closer to those of L-dopa.
Because they take longer to take effect, these drugs are not as useful to relieve symptoms once they have begun.
Dopamine agonists have been shown to relieve symptoms in 70% or more of patients.
- Ropinirole (Requip) was the first drug approved specifically for treatment of moderate-to-severe RLS (more than 15 RLS episodes a month). Side effects are generally mild but may include nausea, vomiting, drowsiness, and dizziness. A small percentage of patients may experience their symptoms worsening and rebound symptoms when the medicine wears off.
- Pramipexole (Mirapex) is also approved for RLS. However, patients may fall asleep, without warning, while taking this drug, even while performing activities such as driving.
- Rotigotine (Neupro) is a patch preparation. Common side effects include back or joint pain, dizziness, decreased appetite, dry mouth, fatigue, sweating, trouble sleeping or upset stomach.
- Cabergoline is a dopamine agonist that should be used only when other medications have been tried and failed; it poses a risk of heart valve damage .
Other dopamine agonists that have tested in small studies include alpha-dihydroergocryptine, or DHEC (Almirid), and piribedil (Trivastal). However, there is not enough evidence to support their use for RLS treatment.
Benzodiazepines
Benzodiazepines, such as clonazepam (Klonopin), are known as sedative hypnotics. Doctors prescribe them for insomnia and anxiety. They may be helpful for RLS that disrupts sleep, especially in younger patients. Clonazepam may be particularly helpful for children with both PLMD and symptoms of attention deficit hyperactivity disorder. The medicine also may be helpful for patients with RLS who are undergoing dialysis.
Side EffectsElderly people are more susceptible to side effects. They should usually start at half the dose prescribed for younger people, and should not take long-acting forms. Side effects may differ depending on whether the benzodiazepine is long-acting or short-acting.
- The drugs may increase depression, a common condition in many people with insomnia.
- Breathing problems may occur with overuse or in people with pre-existing respiratory illness.
- Long-acting drugs have a very high rate of residual daytime drowsiness compared to others. They have been associated with a significantly increased risk for automobile accidents and falls in the elderly, particularly in the first week after taking them. Shorter-acting benzodiazepines do not appear to pose as high a risk.
- There are reports of memory loss (so-called traveler's amnesia), sleepwalking, and odd mood states after taking triazolam (Halcion) and other short-acting benzodiazepines. These effects are rare and probably enhanced by alcohol.
- Because benzodiazepines can cross the placenta and enter breast milk, pregnant and nursing women should not use them. There are some reports of an association between the use of benzodiazepines in the first trimester of pregnancy and the development of cleft lip in newborns. Studies are conflicting at this point, but other side effects are known to occur in babies exposed to these drugs in the uterus.
- In rare cases, overdoses have been fatal.
Benzodiazepines are potentially dangerous when used in combination with alcohol. Some drugs, such as the ulcer medication cimetidine, can slow the breakdown of benzodiazepine.
Withdrawal SymptomsWithdrawal symptoms usually occur after prolonged use and indicate dependence. They can last 1 to 3 weeks after stopping the drug and may include:
- Gastrointestinal distress
- Sweating
- Disturbed heart rhythm
- In severe cases, patients might hallucinate or experience seizures, even a week or more after they stop taking the drug.
Rebound insomnia, which often occurs after withdrawal, typically includes 1 to 2 nights of sleep disturbance, daytime sleepiness, and anxiety. The chances of rebound are higher with the short-acting benzodiazepines than with the longer-acting ones.
Narcotic Pain Relievers
Narcotics are pain-relieving drugs that act on the central nervous system. They are sometimes prescribed for severe cases of RLS. They may be a good choice if pain is a prominent feature. Some evidence also suggests that narcotics reduce the frequency of periodic leg movements.
There are two types of narcotics, both of which have been used for severe RLS:
- Opiates (such as morphine and codeine) come from natural opium. Some patients report relief with the use of the opiate fentanyl (Duragesic), available in skin patch form. An implanted pump that uses morphine and an anesthetic called bupivacaine is showing promise for patients with severe RLS. The pump delivers the drugs to the fluid surrounding the spinal cord (cerebrospinal fluid).
- Opioids are synthetic drugs. The most common example is oxycodone (Percodan, Percocet, Roxicodone, OxyContin, Methadone, and Hydrocodone).
Although the use of narcotics for severe RLS is controversial, some studies have suggested that even when the treatments are long-term, they are rarely addictive for pain sufferers except among patients with a history of substance abuse.
The use of such drugs may be beneficial when included as part of a comprehensive pain management program. Such a program involves screening prospective patients for possible drug abuse, and regularly monitoring those who are taking narcotics. Doses should be adjusted as necessary to achieve an acceptable balance between pain relief and side effects. Patients on long-term opiate therapy should also be monitored periodically for sleep apnea, a condition that causes breathing to stop for short periods many times during the night. Sleep apnea may worsen symptoms of RLS, insomnia, and other complaints.
TramadolTramadol (Ultram) is a pain reliever that has been used as an alternative to opioids. It has opioid-like properties, but is not as addictive. However, there are reports of dependence and abuse with this drug as well. Withdrawal after long-term use (longer than a year) can cause intense symptoms, including diarrhea, insomnia, and even RLS itself.
Antiseizure Drugs
Antiseizure drugs, such as gabapentin (Neurontin), valproic acid (valproate, divalproex, Depakote, Depakene), and carbamazepine (Tegretol) are being tested for RLS. Common side effects included mild sleepiness and dizziness.
Side EffectsAll antiseizure drugs have potentially severe side effects. Therefore, patients should try these medications only after non-drug methods have failed. Side effects of many anti-seizure drugs include nausea, vomiting, heartburn, increased appetite with weight gain, hand tremors, irritability, and temporary hair thinning and hair loss. Taking zinc and selenium supplements may help reduce this last effect. Some anti-seizure drugs can also cause birth defects and, in rare cases, liver toxicity. Gabapentin may have fewer of these side effects than valproic acid or carbamazepine.
Other Drugs
Antidepressants. Bupropion (Wellbutrin), a newer antidepressant, may be helpful for RLS. Bupropion is a weak dopamine reuptake inhibitor, it causes a slight increase in the availability of dopamine in the brain. The drug is not addictive and does not have the severe side effects of other RLS drugs, but more research is needed to determine if it is useful. Clonidine. Clonidine (Catapres), a drug used for high blood pressure, is helpful for some patients and may be an appropriate choice for patients who have RLS accompanied by hypertension. It also may help patients with RLS who are undergoing hemodialysis. Baclofen. The anti-spasm drug baclofen (Lioresal) appears to reduce intensity of RLS (although not frequency of movements). Pregabalin. Pregabalin (Lyrica) is approved for the treatment of diabetic neuropathy, postherpetic neuralgia, and fibromyalgia, and may also be helpful in the treatment of RLS.
Resources
- www.aasmnet.org -- American Academy of Sleep Medicine
- www.sleepfoundation.org -- National Sleep Foundation
- www.ninds.nih.gov -- National Institute of Neurological Disorders and Stroke
- www.nhlbi.nih.gov/about/ncsdr -- National Center on Sleep Disorders Research
- www.rls.org -- Restless Legs Syndrome Foundation
References
AAN Summary of Evidence-based Guideline for Patients and their families. Drug treatments for symptoms of muscle cramps. Available at: www.aan.com/Guidelines/Home/GetGuidelineContent/395 . Accessed 3/8/2016.
Allen RP, Chen C, Garcia-Borreguero D, et al. Comparison of pregabalin with pramipexole for restless legs syndrome. N Engl J Med . 2014 Feb 13;370(7):621-31. PMID: 24521108 www.ncbi.nlm.nih.gov/pubmed/24521108 .
Aurora RN, Kristo DA, Bista SR, et al. Update to the AASM clinical practice guideline: The treatment of restless legs syndrome and periodic limb movement disorder in adults--an update for 2012: practice parameters with an evidence-based systematic review and meta-analyses. Sleep . 2012;35(8):1039-62. PMID: 22851801 www.ncbi.nlm.nih.gov/pubmed/22851801 .
Aurora RN, Kristo DA, Bista SR, et al. Letter to the Editor: Update to the AASM clinical practice guideline: The treatment of restless legs syndrome and periodic limb movement disorder in adults--an update for 2012: practice parameters with an evidence-based systematic review and meta-analyses. Sleep . 2012;35(8):1037. PMID: 22851800 www.ncbi.nlm.nih.gov/pubmed/22851800
Balserak BI, Lee K. Sleep disturbances and sleep-related disorders in pregnancy. In: Kryger MH, Roth T, Dement WC, eds. Principles and Practice of Sleep Medicine . 5 th ed. Philadelphia, PA: Elsevier Saunders; 2011:1572-86.
Bertisch S. In the clinic. Restless legs syndrome. Ann Intern Med . 2015 Nov 3;163(9):ITC1-11. PMID: 26524584 www.ncbi.nlm.nih.gov/pubmed/26524584 .
Chokroverty S, Avidan AY. Sleep and its disorders. In: Daroff RB, Jankovic J, Mazziotta JC, et al., eds. Bradley's Neurology in Clinical Practice . 7th ed. 2016:ch 102;1615-85.
Giorgi L, Asgharian A, Hunter B. Ropinirole in patients with restless legs syndrome and baseline IRLS total scores = 24: efficacy and tolerability in a 26-week, double-blind, parallel group, placebo-controlled study followed by a 40-week open-label extension. Clin Ther . 2013;35(9):1321-36. PMID: 23938061 www.ncbi.nlm.nih.gov/pubmed/23938061 .
Innes KE, Selfe TK, Agarwal P. Prevalence of restless legs syndrome in North American and Western European populations: a systematic review. Sleep Med . 2011 Aug;12(7):623-34. PMID: 21752711 www.ncbi.nlm.nih.gov/pubmed/21752711 .
Lettieri CJ, Eliasson AH. Pneumatic compression devices are an effective therapy for restless legs syndrome: a prospective, randomized, double-blind, sham- controlled trial. Chest . 2009;135(1):74-80. PMID: 19017878 www.ncbi.nlm.nih.gov/pubmed/19017878 .
Ohayon MM, O'Hara R, Vitiello MV. Epidemiology of restless legs syndrome: a synthesis of the literature. Sleep Med Rev . 2012 Aug;16(4):283-95. PMID: 21795081 www.ncbi.nlm.nih.gov/pubmed/21795081 .
Picchietti DL, Bruni O, de Weerd A, et al, International Restless Legs Syndrome Study Group (IRLSSG). Pediatric restless legs syndrome diagnostic criteria: an update by the International Restless Legs Syndrome Study Group. Sleep Med . 2013;14(12):1253-9. PMID: 24184054 www.ncbi.nlm.nih.gov/pubmed/24184054
Picchietti D. Restless legs syndrome: prevalence and impact in children and adolescents--the Peds REST study. Pediatrics . 2007;120(2):253-66. PMID: 17671050 www.ncbi.nlm.nih.gov/pubmed/17671050 .
Ramar K, Olson EJ. Management of common sleep disorders. Am Fam Physician . 2013;88(4):231-8. PMID: 23944726 www.ncbi.nlm.nih.gov/pubmed/23944726 .
Restless Leg Syndrome Foundation. RLS Name Change: Willis-Ekbom Disease. Available online. Last accessed: October 1, 2011.
Silber MH, Becker PM, Earley C, et al. Willis-Ekbom Disease Foundation Revised Consensus Statement on the Management of Restless Legs Syndrome. Mayo Clin Proc . 2013 Sep;88(9):977-86. PMID: 24001490 www.ncbi.nlm.nih.gov/pubmed/24001490 .
Sutton EL. Psychiatric disorders and sleep issues. Med Clin North Am . 2014;98(5):1123-43. Review. PMID: 25134876 www.ncbi.nlm.nih.gov/pubmed/25134876 .
Trenkwalder C, Beneš H, Grote L, , et al. Prolonged release oxycodone-naloxone for treatment of severe restless legs syndrome after failure of previous treatment: a double-blind, randomised, placebo-controlled trial with an open-label extension. Lancet Neurol . 2013;12(12):1141-50. PMID: 24140442 www.ncbi.nlm.nih.gov/pubmed/24140442 .
Trotti LM, Bhadriraju S, Becker LA. Iron for restless legs syndrome. Cochrane Data Base Syst Rev . 2012;16;5:CD007834. PMID: 22592724 www.ncbi.nlm.nih.gov/pubmed/22592724 .
U.S. Food and Drug Administration. FDA approves Horizant to treat restless legs syndrome. FDA News Release, April 7, 2011. Available online. Last accessed September 17, 2011.
U.S. Food and Drug Administration. FDA's MedWatch Safety Alerts: July 2010. Available online. Last Accessed 21 September, 2010.
Wilt TJ, MacDonald R, Ouellette J, et al. Pharmacologic therapy for primary restless legs syndrome: a systematic review and meta-analysis. JAMA Intern Med . 2013 Apr 8;173(7):496-505. PMID: 23460396 www.ncbi.nlm.nih.gov/pubmed/23460396 .
Review Date: 3/9/2016
Reviewed By: Joseph V. Campellone, MD, Division of Neurology, Cooper University Hospital, Camden, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.