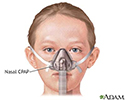
Nasal CPAP
Continuous positive airway pressure; CPAP; Bilevel positive airway pressure; BiPAP; Autotitrating positive airway pressure; APAP; nCPAP; Non-invasive positive pressure ventilation; NIPPV; Non-invasive ventilation; NIV; OSA - CPAP; Obstructive sleep apnea - CPAP
CPAP stands for continuous positive airway pressure. CPAP pumps air under pressure into the airway of the lungs, keeping the windpipe open during sleep. The forced air delivered by CPAP prevents episodes of airway collapse that block the breathing in people with obstructive sleep apnea and other breathing problems.
It is sometimes called nasal continuous positive airflow pressure (nCPAP).
Information
WHO SHOULD USE CPAP
CPAP can successfully treat most people with obstructive sleep apnea . It is safe and works well for people of all ages, including children. If you only have mild sleep apnea and do not feel very sleepy during the day, you may not need it.
Obstructive sleep apnea
Obstructive sleep apnea (OSA) is a problem in which your breathing pauses during sleep. This occurs because of narrowed or blocked airways.

After using CPAP regularly, you may notice:
- Better concentration and memory
- Feeling more alert and less sleepy during the day
- Improved sleep for your bed partner
- Being more productive at work
- Less anxiety and depression and a better mood
- Normal sleep patterns
- Lower blood pressure (in people with high blood pressure)
CPAP works by keeping a steady pressure of forced air in your airway to keep it open. Other devices work in slightly different ways to treat sleep apnea:
- Autotitrating positive airway pressure (APAP) changes pressure throughout the night based on your breathing patterns.
- Bilevel positive airway pressure (BiPAP) has a higher pressure when you breathe in and lower pressure when you breathe out.
BiPAP is useful for children and adults who have:
- Airways that collapse while sleeping, making it hard to breathe freely
- Decreased air exchange in the lung
-
Muscle weakness that makes it difficult to breathe, due to conditions such as
muscular dystrophy
Muscular dystrophy
Muscular dystrophy is a group of inherited disorders that cause muscle weakness and loss of muscle tissue, which get worse over time.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
CPAP or BiPAP may also be used by people who have:
-
Respiratory failure
Respiratory failure
Respiratory acidosis is a condition that occurs when the lungs cannot remove all of the carbon dioxide the body produces. This causes body fluids, e...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Central sleep apnea
Central sleep apnea
Central sleep apnea is a sleep disorder in which breathing stops over and over during sleep.
Read Article Now Book Mark Article -
COPD
COPD
Chronic obstructive pulmonary disease (COPD) is a common lung disease. Having COPD makes it hard to breathe. There are two main forms of COPD:Chroni...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Heart failure
Heart failure
Heart failure is a condition in which the heart is no longer able to pump oxygen-rich blood to the rest of the body efficiently. This causes symptom...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
HOW CPAP WORKS
When using CPAP:
- You wear a mask over your nose or nose and mouth while you sleep.
- The mask is connected by a hose to a small machine that sits at the side of your bed.
- The machine pumps air under pressure through the hose and mask and into your airway while you sleep. This helps keep your airway open.
You may start to use CPAP while you are in the sleep center for the night.
Sleep center
Polysomnography is a sleep study. This test records certain body functions as you sleep, or try to sleep. Polysomnography is used to diagnose sleep...

- Your health care provider will help choose the mask that fits you best.
- They will adjust the settings on the machine while you are asleep.
- The settings will be adjusted based on the severity of your sleep apnea.
If you are using CPAP but your symptoms do not improve, the settings on the machine may need to be changed. Your provider may teach you how to adjust the CPAP at home. Or, you may need to go to the sleep center to have it adjusted.
GETTING USED TO THE DEVICE
It can take time to get used to using a CPAP device. The first few nights of CPAP therapy are often the hardest. You may not sleep well at the start of treatment.
If you are having problems, you may be tempted not to use CPAP for the whole night. But, you will get used to it more quickly if you use the machine for the entire night.
When using CPAP for the first time, you may have:
- A feeling of being closed in (claustrophobia)
- Chest muscle discomfort, which usually goes away after awhile
- Eye irritation
- Redness and sores over the bridge of your nose
- Runny or stuffed-up nose
- Sore or dry mouth
- Nosebleeds
- Upper respiratory infections
Many of these problems can be helped or prevented.
- Ask your doctor or therapist about using a mask that is lightweight and cushioned. Some masks are used only around or inside the nostrils.
- Make sure the mask fits correctly so that it does not leak air. It should not be too tight or too loose.
- Try nasal salt water sprays for a stuffed nose.
- Use a humidifier to help with dry skin or nasal passages.
- Keep your CPAP equipment clean.
- Place your CPAP machine underneath your bed to limit noise.
- Most machines are quiet, but if you notice sounds that make it hard to sleep, tell your doctor or therapist.
Your doctor or therapist can lower the pressure on the CPAP machine and then increase it again at a slow pace. Some new machines can automatically adjust to the pressure that is needed.
References
Buchanan P, Grunstein R. Positive airway pressure treatment for obstructive sleep apnea-hypopnea syndrome. In: Kryger MH, Roth T, Dement WC. Principles and Practice of Sleep Medicine . 5th ed. Philadelphia, PA: Elsevier Saunders; 2011:chap 107.
Kimoff JR. Obstructive sleep apnea. In: Broaddus VC, Mason RJ, Ernst JD, et al, eds. Murray and Nadel's Textbook of Respiratory Medicine . 6th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 88.
Qaseem A, Holty JE, Owens DK, et al., Clinical Guidelines Committee of the American College of Physicians. Management of obstructive sleep apnea in adults: A clinical practice guideline from the American College of Physicians. Ann Intern Med . 2013;159:471-83. PMID: 24061345 www.ncbi.nlm.nih.gov/pubmed/24061345 .
Review Date: 10/20/2015
Reviewed By: Allen J. Blaivas, DO, Division of Pulmonary, Critical Care, and Sleep Medicine, VA New Jersey Health Care System, Clinical Assistant Professor, Rutger's New Jersey Medical School, East Orange, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.