Vaginal yeast infection
Yeast infection - vagina; Vaginal candidiasis; Monilial vaginitis
Vaginal yeast infection is an infection of the vagina. It is most commonly due to the fungus Candida albicans .
Causes
Most women have a vaginal yeast infection at some time. Candida albicans is a common type of fungus. It is often found in small amounts in the vagina , mouth, digestive tract, and on the skin. Most of the time, it does not cause infection or symptoms.
Vagina
The vagina is the female body part that connects the womb (uterus) and cervix to the outside of the body.

Candida and the many other germs that normally live in the vagina keep each other in balance. However, sometimes the number of Candida increases, leading to a yeast infection.
This can happen if:
- You are taking antibiotics used to treat another infection. Antibiotics change the normal balance between germs in the vagina.
- You are pregnant
- You are obese
-
You have
diabetes
Diabetes
Diabetes is a chronic disease in which the body cannot regulate the amount of sugar in the blood.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
A yeast infection is not spread through sexual contact. However, some men will develop symptoms such as itching and a rash on the penis after having sexual contact with an infected partner.
Itching
Itching is a tingling or irritation of the skin that makes you want to scratch the area. Itching may occur all over the body or only in one location...

Rash
Rashes involve changes in the color, feeling or texture of your skin.

Having many vaginal yeast infections may be a sign of other health problems. Other vaginal infections and discharges can be mistaken for a vaginal yeast infection.
Symptoms
Symptoms include:
-
Abnormal vaginal discharge
. Discharge can range from slightly watery, white discharge to thick, white, and chunky (like cottage cheese).
Abnormal vaginal discharge
Vaginal discharge refers to secretions from the vagina. The discharge may be:Thick, pasty, or thinClear, cloudy, bloody, white, yellow, or greenOdor...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Itching and burning of the vagina and labia
- Pain with intercourse
-
Painful urination
Painful urination
Painful urination is any pain, discomfort, or burning sensation when passing urine.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Redness and swelling of the skin just outside of the vagina (vulva)
Exams and Tests
You will have a pelvic exam. It may show:
-
Swelling and redness of the skin of the
vulva
, in the
vagina
, and on the cervix
Vulva
The vulva is made up of the female genital parts that are outside the body. It includes the "lips" or folds of skin (labia), clitoris, and the openi...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleVagina
The vagina is the female body part that connects the womb (uterus) and cervix to the outside of the body.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Dry, white spots on the vaginal wall
- Cracks in the skin of the vulva.
A small amount of the vaginal discharge is examined using a microscope. This is called a wet mount and KOH test.
Vaginal discharge
Vaginal discharge refers to secretions from the vagina. The discharge may be:Thick, pasty, or thinClear, cloudy, bloody, white, yellow, or greenOdor...

Wet mount
The vaginitis wet mount test is a test to detect an infection of the vagina.

Sometimes, a culture is taken when the infection does not get better with treatment or comes back many times.
Your health care provider may order other tests to rule out other causes of your symptoms.
Treatment
Medicines to treat vaginal yeast infections are available as creams, ointments, vaginal tablets or suppositories and oral tablets. Most can be bought without needing to see your provider.
Treating yourself at home is probably OK if:
- Your symptoms are mild and you do not have pelvic pain or a fever
- This is not your first yeast infection and you have not had many yeast infections in the past
- You are not pregnant
- You are not worried about other sexually transmitted infections from recent sexual contact
Medicines you can buy yourself to treat a vaginal yeast infection are:
- Miconazole
- Clotrimazole
- Tioconazole
- Butoconazole
When using these medicines:
- Read the packages carefully and use them as directed.
- You will need to take the medicine for 1 to 7 days, depending on which medicine you buy. (If you do not get repeated infections, a 1-day medicine might work for you.)
- Do not stop using these medicines early because your symptoms are better.
You doctor can also prescribe a pill that you only take by mouth once.
If your symptoms are worse or you get vaginal yeast infections often, you may need:
- Medicine for up to 14 days
- Clotrimazole vaginal suppository or fluconazole pill every week to prevent new infections
To help prevent and treat vaginal discharge:
- Keep your genital area clean and dry. Avoid soap and rinse with water only. Sitting in a warm, but not hot, bath may help your symptoms.
- Avoid douching. Although many women feel cleaner if they douche after their period or intercourse, it may worsen vaginal discharge. Douching removes healthy bacteria lining the vagina that protect against infection.
- Eat yogurt with live cultures or take Lactobacillus acidophilus tablets when you are on antibiotics. This may help to prevent a yeast infection.
- Use condoms to avoid catching or spreading other infections.
- Avoid using feminine hygiene sprays, fragrances, or powders in the genital area.
- Avoid wearing tight-fitting pants or shorts, which may cause irritation.
- Wear cotton underwear or cotton-crotch pantyhose. Avoid underwear made of silk or nylon, because they can increase sweating in the genital area, which leads to growth of more yeast.
- Keep your blood sugar level under good control if you have diabetes.
- Avoid wearing wet bathing suits or exercise clothing for long periods of time. Wash sweaty or wet clothes after each use.
Outlook (Prognosis)
Most of the time, symptoms go away completely with proper treatment.
Possible Complications
A lot of scratching may cause the skin to crack, making you more likely to get a skin infection.
Repeat infections that occur right after treatment, or a yeast infection that does not respond well to treatment, may be an early sign of diabetes or rarely, HIV.
When to Contact a Medical Professional
Call your provider if:
- This is the first time that you have had symptoms of a vaginal yeast infection.
- You are not sure if you have a yeast infection.
- Your symptoms don't go away after using over-the-counter medicines.
- Your symptoms get worse.
- You develop other symptoms.
- You may have been exposed to an STD.
References
Eckert LO, Lentz GM. Infections of the lower genital tract. In: Lentz GM, Lobo RA, Gershenson DM, Katz VL, eds. Comprehensive Gynecology . 6th ed. Philadelphia, PA: Elsevier Mosby; 2012:chap 23.
Habif TP. Superficial fungal infections. In: Habif TP, ed. Clinical Dermatology . 6th ed. St. Louis, MO: Elsevier; 2016:chap 13.
Hoefgen HR, Merritt DF. Vulvovaginitis. In: Kliegman RM, Stanton BF, St Geme JW, Schor NF, eds. Nelson Textbook of Pediatrics . 20th ed. Philadelphia, PA: Elsevier; 2016:chap 549.
Kauffman CA. Candidiasis. In: Goldman L, Schafer AI, eds. Goldman's Cecil Medicine . 25th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 338.
-
Candida, fluorescent stain - illustration
This microscopic film shows a fluorescent stain of Candida. Candida is a yeast (fungus) that causes mild disease, but in immunocompromised individuals it may cause life-threatening illness. (Image courtesy of the Centers for Disease Control and Prevention.)
Candida, fluorescent stain
illustration
-
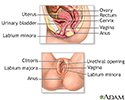
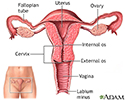
Female reproductive anatomy - illustration
External structures of the female reproductive anatomy include the labium minora and majora, the vagina and the clitoris. Internal structures include the uterus, ovaries and cervix.
Female reproductive anatomy
illustration
-
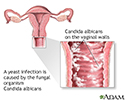
Yeast infections - illustration
Yeast infections may follow a course of antibiotics that were prescribed for another purpose. The antibiotics change the normal "balance" between organisms in the vagina by suppressing the growth of protective bacteria that normally have an antifungal effect.
Yeast infections
illustration
-
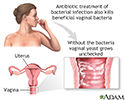
Secondary infection - illustration
Secondary infection occurs during or after treatment of a primary infection because the normal bacterial flora is destroyed, allowing yeast to flourish.
Secondary infection
illustration
-
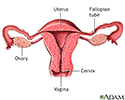
Uterus - illustration
The uterus is a hollow muscular organ located in the female pelvis between the bladder and rectum. The ovaries produce the eggs that travel through the fallopian tubes. Once the egg has left the ovary it can be fertilized and implant itself in the lining of the uterus. The main function of the uterus is to nourish the developing fetus prior to birth.
Uterus
illustration
-
Normal uterine anatomy (cut section) - illustration
The uterus is a muscular organ with thick walls, two upper openings to the fallopian tubes and an inferior opening to the vagina.
Normal uterine anatomy (cut section)
illustration
-
Candida, fluorescent stain - illustration
This microscopic film shows a fluorescent stain of Candida. Candida is a yeast (fungus) that causes mild disease, but in immunocompromised individuals it may cause life-threatening illness. (Image courtesy of the Centers for Disease Control and Prevention.)
Candida, fluorescent stain
illustration
-
Female reproductive anatomy - illustration
External structures of the female reproductive anatomy include the labium minora and majora, the vagina and the clitoris. Internal structures include the uterus, ovaries and cervix.
Female reproductive anatomy
illustration
-
Yeast infections - illustration
Yeast infections may follow a course of antibiotics that were prescribed for another purpose. The antibiotics change the normal "balance" between organisms in the vagina by suppressing the growth of protective bacteria that normally have an antifungal effect.
Yeast infections
illustration
-
Secondary infection - illustration
Secondary infection occurs during or after treatment of a primary infection because the normal bacterial flora is destroyed, allowing yeast to flourish.
Secondary infection
illustration
-
Uterus - illustration
The uterus is a hollow muscular organ located in the female pelvis between the bladder and rectum. The ovaries produce the eggs that travel through the fallopian tubes. Once the egg has left the ovary it can be fertilized and implant itself in the lining of the uterus. The main function of the uterus is to nourish the developing fetus prior to birth.
Uterus
illustration
-
Normal uterine anatomy (cut section) - illustration
The uterus is a muscular organ with thick walls, two upper openings to the fallopian tubes and an inferior opening to the vagina.
Normal uterine anatomy (cut section)
illustration
-
Candidiasis
(Alt. Medicine)
Review Date: 11/5/2015
Reviewed By: Cynthia D. White, MD, Fellow American College of Obstetricians and Gynecologists, Group Health Cooperative, Bellevue, WA. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.