Spinal cord trauma
Spinal cord injury; Compression of spinal cord; SCI; Cord compression
Spinal cord trauma is damage to the spinal cord. It may result from direct injury to the cord itself or indirectly from disease of the nearby bones, tissues, or blood vessels.
Causes
The spinal cord contains the nerves. These nerves carry messages between your brain and body. The cord passes through your neck and back down to the first lumbar vertebra.
Spinal cord injury (SCI) can be caused by any of the following:
- Assault
- Falls
- Gunshot wounds
- Industrial accidents
- Motor vehicle accidents
- Sports injuries
A minor injury can damage the spinal cord. Conditions, such as rheumatoid arthritis or osteoporosis can weaken the spinal cord. Injury can also occur if the spinal canal protecting the spinal cord has become too narrow ( spinal stenosis ). This occurs during normal aging.
Rheumatoid arthritis
Rheumatoid arthritis (RA) is a long-term disease. It leads to inflammation of the joints and surrounding tissues. It can also affect other organs....

Osteoporosis
Osteoporosis is a disease in which bones become fragile and more likely to break (fracture).

Spinal stenosis
Spinal stenosis is narrowing of the spinal column that causes pressure on the spinal cord, or narrowing of the openings (called neural foramina) wher...

Direct injury or damage to the spinal cord can occur due to:
- Bruises if the bones or disks have been weakened
- Fragments of bone (such as from broken vertebrae, which are the spine bones) in the spinal cord
- Fragments of metal (such as from a traffic accident or gunshot)
- Sideway pulling or pressing or compression from twisting of the head, neck or back during an accident or intense chiropractic manipulation
Bleeding, fluid buildup, and swelling can occur inside or outside the spinal cord (but within the spinal canal). This can press on the spinal cord and damage it.
Most high impact SCIs, such as from motor vehicle accidents or sports injuries, are seen in young, healthy people. Men ages 15 to 35 are most often affected.
Risk factors include:
- Participating in risky physical activities
- Riding in or on high-speed vehicles
- Diving into shallow water
Low impact SCI often occurs in older adults from falls while standing or sitting. Injury is due to a weakened spine from aging or bone loss ( osteoporosis ).
Osteoporosis
Osteoporosis is a disease in which bones become fragile and more likely to break (fracture).

Symptoms
Symptoms vary, depending on the location of the injury. SCI causes weakness and loss of feeling at, and below the injury. How severe the symptoms are depends on whether the entire cord is severely injured (complete) or only partially injured (incomplete).
An injury at and below the first lumbar vertebra does not cause SCI. But, it may cause cauda equina syndrome. This is an injury to the nerve roots in this area. This is a medical emergency and needs surgery right away.
Injuries of the spinal cord at any level can cause:
- Increased muscle tone (spasticity)
- Loss of normal bowel and bladder control (may include constipation, incontinence, bladder spasms)
- Numbness
- Sensory changes
- Pain
- Weakness, paralysis
CERVICAL (NECK) INJURIES
When spinal cord injuries are in the neck area, symptoms can affect the arms, legs, and middle of the body. The symptoms:
- May occur on 1 or both sides of the body
- Can include breathing problems from paralysis of the breathing muscles, if the injury is high up in the neck
THORACIC (CHEST LEVEL) INJURIES
When spinal injuries are at chest level, symptoms can affect the legs. Injuries to the cervical or high thoracic spinal cord may also result in:
- Blood pressure problems
- Abnormal sweating
- Trouble maintaining normal temperature
LUMBAR SACRAL (LOWER BACK) INJURIES
When spinal injuries are at the lower back level, symptoms can affect one or both legs. Muscles that control the bowels and bladder can also be affected. Spine injuries can damage the spinal cord if they are at the upper portion of the lumbar spine or the nerve roots if they are at the lower lumbar spine.
Exams and Tests
SCI is a medical emergency that needs medical attention right away.
The health care provider will perform a physical exam, including a brain and nervous system (neurological) exam. This will help identify the exact location of the injury, if it is not known.
Some of the reflexes may be abnormal or missing. Once swelling goes down, some reflexes may slowly recover.
Reflexes
A reflex is a muscle reaction that happens automatically in response to stimulation. Certain sensations or movements produce specific muscle respons...

Tests that may be ordered include:
-
CT
scan or MRI of the spine
CT
A computed tomography (CT) scan is an imaging method that uses x-rays to create pictures of cross-sections of the body. Related tests include:Abdomin...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Myelogram
(an x-ray of the spine after injecting dye)
Myelogram
A lumbosacral spine x-ray is a picture of the small bones (vertebrae) in the lower part of the spine. This area includes the lumbar region and the s...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Spine x-rays
Spine x-rays
A thoracic spine x-ray is an x-ray of the twelve chest (thoracic) bones (vertebrae). The vertebrae are separated by flat pads of cartilage called di...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Electromyography
(EMG)
Electromyography
Electromyography (EMG) is a test that checks the health of the muscles and the nerves that control the muscles.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Nerve conduction studies
Nerve conduction studies
Nerve conduction velocity (NCV) is a test to see how fast electrical signals move through a nerve.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Treatment
An SCI needs to be treated right away. The time between the injury and treatment can affect the outcome.
Medicines called corticosteroids are sometimes used to reduce swelling that may damage the spinal cord, though there is no clear evidence that they are useful.
If spinal cord pressure is caused by a growth that can be removed or reduced before the spinal nerves are completely destroyed, paralysis may improve.
Paralysis
Muscle function loss is when a muscle does not work or move normally. The medical term for complete loss of muscle function is paralysis.
Surgery may be needed to:
- Realign the spinal bones (vertebrae)
-
Remove fluid or tissue that presses on the spinal cord (decompression
laminectomy
)
Laminectomy
Laminectomy is surgery to remove the lamina. This is part of the bone that makes up a vertebra in the spine. Laminectomy may also be done to remove...
Read Article Now Book Mark Article - Remove bone fragments, disk fragments, or foreign objects
- Fuse broken spinal bones or place spinal braces
Bed rest may be needed to allow the bones of the spine to heal.
Spinal traction may be suggested. This can help keep the spine from moving. The skull may be held in place with tongs. These are metal braces placed in the skull and attached to weights or to a harness on the body (halo vest). You may need to wear the spine braces for many months.
Traction
Traction means pulling on part of the body. Most often, traction uses devices such as weights and pulleys to put tension on a displaced bone or joint...
The health care team will also tell you what to do for muscle spasms and bowel and bladder dysfunction. They will also teach you how to care for your skin and protect it from pressure sores.
Muscle spasms
Muscle cramps are when a muscle gets tight (contracts) without you trying to tighten it, and it does not relax. Cramps may involve all or part of on...

You will probably need physical therapy, occupational therapy, and other rehabilitation after the injury has healed. Rehabilitation will help you cope with the disability from your SCI.
Support Groups
Seek out organizations for additional information on SCI. They can provide support as you recover.
Organizations
The following organizations are good resources for information on spinal injury:National Institute of Neurological Disorders and Stroke -- www. ninds...
Outlook (Prognosis)
How well a person does depends on the level of injury. Injuries in the upper spine lead to more disability than injuries in the lower spine.
Paralysis and loss of sensation of part of the body are common. This includes total paralysis or numbness, and loss of movement and feeling. Death is possible, especially if there is paralysis of the breathing muscles.
Loss of sensation
Numbness and tingling are abnormal sensations that can occur anywhere in your body, but they are often felt in your fingers, hands, feet, arms, or le...

A person who recovers some movement or feeling within 1 week usually has a good chance of recovering more function, although this may take 6 months or more. Losses that remain after 6 months are more likely to be permanent.
Routine bowel care often takes 1 hour or more each day. Most people with SCI must perform bladder catheterization regularly.
The person's home will usually need to be modified.
Most people with SCI are in a wheelchair or need assistive devices to get around.
Possible Complications
The following are possible complications of SCI:
-
Blood pressure changes that can be extreme (
autonomic hyperreflexia
)
Autonomic hyperreflexia
Autonomic dysreflexia is an abnormal, overreaction of the involuntary (autonomic) nervous system to stimulation. This reaction may include: Change i...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Increased risk for injury to numb areas of the body
-
Increased risk for
urinary tract infections
Urinary tract infections
A urinary tract infection, or UTI, is an infection of the urinary tract. The infection can occur at different points in the urinary tract, including...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Long-term kidney disease
Long-term kidney disease
Chronic kidney disease is the slow loss of kidney function over time. The main job of the kidneys is to remove wastes and excess water from the body...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Loss of bladder
and
bowel control
Loss of bladder
Urinary (or bladder) incontinence happens when you are not able to keep urine from leaking out of your urethra. The urethra is the tube that carries...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleBowel control
Bowel incontinence is the loss of bowel control, causing you to pass stool unexpectedly. This can range from sometimes leaking a small amount of sto...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Loss of sexual function
- Paralysis of breathing muscles and limbs (paraplegia, quadriplegia)
- Pressure sores
-
Problems due to not being able to move, such as
deep vein thrombosis
, lung infections, skin breakdown, and muscle stiffness
Deep vein thrombosis
Deep vein thrombosis (DVT) is a condition that occurs when a blood clot forms in a vein deep inside a part of the body. It mainly affects the large ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Shock
Shock
Shock is a life-threatening condition that occurs when the body is not getting enough blood flow. Lack of blood flow means that the cells and organs...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
People living at home with SCI should do the following to prevent complications:
- Get lung (pulmonary) care each day (if they need it).
- Follow all instructions for bladder care to avoid infections and damage to the kidneys.
- Follow all instructions for routine wound care to avoid pressure sores.
-
Keep
immunizations
up to date.
Immunizations
Vaccines are used to boost your immune system and prevent serious, life-threatening diseases.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Maintain routine health visits with their doctor.
When to Contact a Medical Professional
Call your provider if you have a back or neck injury. Call 911 if you lose movement or feeling. This is a medical emergency.
Managing SCI begins at the site of an accident. Trained paramedics immobilize the injured spine to prevent further nervous system damage.
Someone who may have a SCI should not be moved unless they are in immediate danger.
Prevention
The following measures may help prevent SCIs:
- Proper safety practices during work and play can prevent many spinal cord injuries. Use protective equipment for any activity in which an injury is possible.
- Diving into shallow water is a major cause of spinal cord trauma. Check water depth before diving, and look for rocks or other possible objects in the way.
- Football and sledding can often involve sharp blows or abnormal twisting and bending of the back or neck, which can cause SCI. Before sledding down a hill, check the area for obstacles. Use the right techniques and equipment when playing football or other contact sports.
- Defensive driving and wearing a seat belt reduces the risk of serious injury if there is a car accident.
- Install and use handrails in the bathroom.
- People who have poor balance may need to use a walker or cane.
References
Arora S, Flower OJ. Spinal injuries. In: Bersten AD, Soni N, eds. Oh's Intensive Care Manual . 7th ed. Philadelphia, PA: Elsevier; 2014:chap 78.
Bryce TN. Spinal cord injury. In: Cifu DX, ed. Braddom's Physical Medicine and Rehabilitation . 5th ed. Philadelphia, PA: Elsevier; 2016:chap 49.
Dalzell K, Nouri A, Fehlings MG. The timing of management of spinal cord injuries. In: Browner BD, Jupiter JB, Krettek C, Anderson PA, eds. Skeletal Trauma: Basic Science, Management, and Reconstruction . 5th ed. Philadelphia, PA: Elsevier Saunders; 2015:chap 32.
Kaji AH, Newton EJ, Hockberger RS. Spinal injuries. In: Marx JA, Hockberger RS, Walls RM, et al, eds. Rosen's Emergency Medicine . 8th ed. Philadelphia, PA: Elsevier Saunders; 2014:chap 43.
Snyder LA, Tan L, Gerard C, Fessler RG. Spinal cord trauma. In: Daroff RB, Jankovic J, Mazziotta JC, Pomeroy SL, eds. Bradley's Neurology in Clinical Practice . 7th ed. Philadelphia, PA: Elsevier; 2016:chap 63.
-
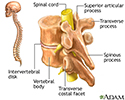
Vertebrae - illustration
The vertebral column is made up of 26 bones that provide axial support to the trunk. The vertebral column provides protection to the spinal cord, which runs through its central cavity. Between each vertebra is an intervertebral disk, which acts as a shock absorber.
Vertebrae
illustration
-
Cauda equina - illustration
The spinal cord ends in the lumbar area and continues through the vertebral canal as spinal nerves. Because of its resemblance to a horse's tail, the collection of these nerves at the end of the spinal cord is called the cauda equina. These nerves send and receive messages to and from the lower limbs and pelvic organs.
Cauda equina
illustration
-
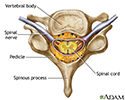
Vertebra and spinal nerves - illustration
The spinal cord and its peripheral nerves are protected by the vertebral column, a stack of bones which surround and provide support. Between the vertebrae is a fluid-filled disk.
Vertebra and spinal nerves
illustration
-
Vertebrae - illustration
The vertebral column is made up of 26 bones that provide axial support to the trunk. The vertebral column provides protection to the spinal cord, which runs through its central cavity. Between each vertebra is an intervertebral disk, which acts as a shock absorber.
Vertebrae
illustration
-
Cauda equina - illustration
The spinal cord ends in the lumbar area and continues through the vertebral canal as spinal nerves. Because of its resemblance to a horse's tail, the collection of these nerves at the end of the spinal cord is called the cauda equina. These nerves send and receive messages to and from the lower limbs and pelvic organs.
Cauda equina
illustration
-
Vertebra and spinal nerves - illustration
The spinal cord and its peripheral nerves are protected by the vertebral column, a stack of bones which surround and provide support. Between the vertebrae is a fluid-filled disk.
Vertebra and spinal nerves
illustration
Review Date: 5/9/2016
Reviewed By: Luc Jasmin, MD, PhD, FRCS (C), FACS, Department of Surgery at Providence Medical Center, Medford OR; Department of Surgery at Ashland Community Hospital, Ashland OR; Department of Maxillofacial Surgery at UCSF, San Francisco, CA. Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.