Spinal muscular atrophy
Werdnig-Hoffmann disease; Kugelberg-Welander disease
Spinal muscular atrophy is a group of disorders of the motor neurons (motor cells). These disorders are passed down through families (inherited) and can appear at any stage of life. The disorder leads to muscle weakness and atrophy.
Causes
Spinal muscular atrophy (SMA) is a collection of different motor nerve diseases. Grouped together, it is the second leading cause of hereditary neuromuscular disease, after Duchenne muscular dystrophy .
Duchenne muscular dystrophy
Duchenne muscular dystrophy is an inherited disorder. It involves muscle weakness, which quickly gets worse.

Most of the time, a person must get the defective gene from both parents to be affected. The most severe form is SMA type I, also called Werdnig-Hoffman disease. Infants with SMA type II have less severe symptoms during early infancy, but they become weaker with time. SMA type III is a less severe form of the disease.
In rare cases, SMA begins in adulthood. This is the mildest form of the disease.
A family history of spinal muscular atrophy in an immediate family member (such as brother or sister) is a risk factor for all types of the disorder.
Symptoms
Symptoms of SMA are:
- Infants with SMA type I are born with very little muscle tone, weak muscles, and feeding and breathing problems.
- With SMA type II, symptoms may not appear until age 6 months to 2 years.
- Type III SMA is a milder disease that starts in childhood or adolescence and slowly gets worse.
- Type IV is even milder, with weakness starting in adulthood.
Often, weakness is first felt in the shoulder and leg muscles. Weakness gets worse over time and eventually becomes severe.
Symptoms in an infant:
- Breathing difficulty, leading to a lack of oxygen
- Feeding difficulty (food may go into the windpipe instead of the stomach)
- Floppy infant (poor muscle tone)
- Lack of head control
- Little movement
- Weakness that gets worse
Symptoms in a child:
- Frequent, increasingly severe respiratory infections
- Nasal speech
- Posture that gets worse
With SMA, the nerves that control feeling (sensory nerves) are not affected. So, a person with the disease can feel things normally.
Exams and Tests
The health care provider will take a careful history and perform a brain/nervous system (neurologic) examination to find out if there is:
- A family history of neuromuscular disease
- Floppy (flaccid) muscles
- No deep tendon reflexes
- Twitches of the tongue muscle
Tests that may be ordered include:
-
Aldolase
blood test
Aldolase
Aldolase is a protein (called an enzyme) that helps break down certain sugars to produce energy. It is found in high amount in muscle tissue. A test...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Erythrocyte sedimentation rate
(ESR)
Erythrocyte sedimentation rate
ESR stands for erythrocyte sedimentation rate. It is commonly called a "sed rate. "It is a test that indirectly measures how much inflammation is in...
Read Article Now Book Mark Article -
Creatine phosphate kinase blood test
Creatine phosphate kinase blood test
Creatine phosphokinase (CPK) is an enzyme in the body. It is found mainly in the heart, brain, and skeletal muscle. This article discusses the test...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - DNA testing to confirm diagnosis
-
Electromyography
(EMG)
Electromyography
Electromyography (EMG) is a test that checks the health of the muscles and the nerves that control the muscles.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Lactate/pyruvate
-
MRI of the spine
MRI of the spine
A magnetic resonance imaging (MRI) scan is an imaging test that uses powerful magnets and radio waves to create pictures of the body. It does not us...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Muscle biopsy
Muscle biopsy
A muscle biopsy is the removal of a small piece of muscle tissue for examination.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Nerve conduction
Nerve conduction
Nerve conduction velocity (NCV) is a test to see how fast electrical signals move through a nerve.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Amino acid blood tests
-
Thyroid-stimulating hormone
(TSH) blood test
Thyroid-stimulating hormone
A TSH test measures the amount of thyroid stimulating hormone (TSH) in your blood. TSH is produced by the pituitary gland. It tells the thyroid gla...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Treatment
There is no treatment to cure the weakness caused by the disease. Supportive care is important. Breathing complications are common in the more severe forms of SMA. To help with breathing, a device or machine called a ventilator may be needed.
People with SMA also need to be watched for choking. This is because the muscles that control swallowing are weak.
Physical therapy is important to prevent contractions of muscles and tendons and abnormal curvature of the spine ( scoliosis ). Bracing may be needed. Surgery may be needed to correct skeletal deformities, such as scoliosis.
Scoliosis
Scoliosis is an abnormal curving of the spine. Your spine is your backbone. It runs straight down your back. Everyone's spine naturally curves a b...

Outlook (Prognosis)
Children with SMA type I rarely live longer than 2 to 3 years because of respiratory problems and infections. Survival time with type II is longer, but the disease kills most of those who are affected while they are still children.
Children with type III disease may survive into early adulthood. But, people with all forms of the disease have weakness and debility that gets worse over time. Adults who develop SMA often have a normal life expectancy.
Possible Complications
Complications that may result from SMA include:
-
Aspiration
(food and fluids get into the lungs, causing pneumonia)
Aspiration
Aspiration means to draw in or out using a sucking motion. It has two meanings:Breathing in a foreign object (sucking food into the airway). A medic...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Contractions of muscles and tendons
- Heart failure
- Scoliosis
When to Contact a Medical Professional
Call your provider if your child:
- Appears weak
- Develops any other symptoms of spinal muscular atrophy
- Has difficulty feeding
Breathing difficulty can rapidly become an emergency condition.
Breathing difficulty
Breathing difficulty may involve:Difficult breathingUncomfortable breathingFeeling like you are not getting enough air

Prevention
Genetic counseling is recommended for people with a family history of spinal muscular atrophy who want to have children.
References
Darras BT, Markowitz JA, Monani UR, De Vivo DC. Spinal muscular atrophies. In: Darras BT, Jones R, Ryan MM, De Vivo DC, eds. Neuromuscular Disorders of Infancy, Childhood, and Adolescence . 2nd ed. Philadelphia, PA: Elsevier; 2015:chap 8.
Rudnik-Schoneborn S, Zerres K. Spinal muscular atrophies. In: Rimoin DL, Korf BR, Connor JM, Pyeritz RE, eds. Emery and Rimoin's Principles and Practice of Medical Genetics . 6th ed. Philadelphia, PA: Elsevier; 2013:chap 128.
-
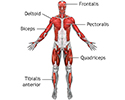
Superficial anterior muscles - illustration
Superficial muscles are close to the surface of the skin. Muscles which lie closer to bone or internal organs are called deep muscles.
Superficial anterior muscles
illustration
-
Scoliosis - illustration
Abnormal curvature in the spine is known as scoliosis, and generally begins just at the onset of puberty and progresses during the period of rapid growth. Most junior high schools routinely screen for scoliosis because, if caught early, progressive spine curvature can be prevented. Scoliosis affects girls much more frequently than boys.
Scoliosis
illustration
-
Superficial anterior muscles - illustration
Superficial muscles are close to the surface of the skin. Muscles which lie closer to bone or internal organs are called deep muscles.
Superficial anterior muscles
illustration
-
Scoliosis - illustration
Abnormal curvature in the spine is known as scoliosis, and generally begins just at the onset of puberty and progresses during the period of rapid growth. Most junior high schools routinely screen for scoliosis because, if caught early, progressive spine curvature can be prevented. Scoliosis affects girls much more frequently than boys.
Scoliosis
illustration
Review Date: 1/5/2016
Reviewed By: Joseph V. Campellone, MD, Division of Neurology, Cooper University Hospital, Camden, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.