Multiple system atrophy
Shy-Drager syndrome; Neurologic orthostatic hypotension; Shy-McGee-Drager syndrome; Parkinson plus syndrome; MSA-P; MSA-C
Multiple system atrophy (MSA) is a rare condition that causes symptoms similar to Parkinson disease . However, people with MSA have more widespread damage to the part of the nervous system that controls important functions such as heart rate, blood pressure, and sweating.
Parkinson disease
Parkinson disease causes certain brain cells to die. These are the cells that help control movement and coordination. The disease leads to shaking ...

Causes
The cause is unknown. MSA develops gradually and is most often diagnosed in men older than 60.
Symptoms
MSA damages the nervous system. Symptoms may include:
- Face changes, such as a masklike appearance to the face and staring
- Difficulty chewing or swallowing (occasionally), not able to close the mouth
- Disrupted sleep patterns (often during rapid eye movement [REM] sleep late at night)
-
Dizziness
or
fainting
when standing up or after standing still
Dizziness
Dizziness is a term that is often used to describe 2 different symptoms: lightheadedness and vertigo. Lightheadedness is a feeling that you might fai...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleFainting
Fainting is a brief loss of consciousness due to a drop in blood flow to the brain. The episode most often lasts less than a couple of minutes and y...
Read Article Now Book Mark Article - Frequent falls
-
Erection problems
Erection problems
An erection problem occurs when a man cannot get or keep an erection that is firm enough for intercourse. You may not be able to get an erection at ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Loss of control over bowels or bladder
- Problems with activity that requires small movements (loss of fine motor skills), such as writing that is small and hard to read
- Loss of sweating in any part of the body
- Mild decline in mental function
-
Movement difficulties
, such as loss of balance, shuffling when walking
Movement difficulties
Uncoordinated movement is due to a muscle control problem that causes an inability to coordinate movements. It leads to a jerky, unsteady, to-and-fr...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Muscle aches and pains (myalgia), and stiffness
- Nausea and problems with digestion
- Posture problems, such as unstable, stooped, or slumped over
- Slow movements
- Tremors
-
Vision changes
, decreased or blurred vision
Vision changes
There are many types of eye problems and vision disturbances, such as: HalosBlurred vision (the loss of sharpness of vision and the inability to see ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Voice and speech changes
Other symptoms that may occur with this disease:
-
Confusion
Confusion
Confusion is the inability to think as clearly or quickly as you normally do. You may feel disoriented and have difficulty paying attention, remembe...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Dementia
Dementia
Dementia is a loss of brain function that occurs with certain diseases. It affects memory, thinking, language, judgment, and behavior.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Depression
Depression
Depression may be described as feeling sad, blue, unhappy, miserable, or down in the dumps. Most of us feel this way at one time or another for shor...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Sleep-related breathing difficulties, including
sleep apnea
or a blockage in the air passage that leads to a harsh vibrating sound
Sleep apnea
Obstructive sleep apnea (OSA) is a problem in which your breathing pauses during sleep. This occurs because of narrowed or blocked airways.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Exams and Tests
Your health care provider will examine you, and check your eyes, nerves, and muscles.
Your blood pressure will be taken while you are lying down and standing up.
There are no specific tests to confirm this disease. A doctor who specializes in the nervous system (neurologist) can make the diagnosis based on:
- History of symptoms
- Physical examination results
- Ruling out other causes of symptoms
Testing to help confirm the diagnosis may include:
-
MRI of head
MRI of head
A head MRI (magnetic resonance imaging) is an imaging test that uses powerful magnets and radio waves to create pictures of the brain and surrounding...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Plasma
norepinephrine
levels
Norepinephrine
This test measures the levels of catecholamines in the blood. Catecholamines are hormones made by the adrenal glands. Catecholamines are more often...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Urine examination for norepinephrine breakdown products (
urine catecholamines
)
Urine catecholamines
Catecholamines are chemicals made by nerve tissue (including the brain) and the adrenal gland. The main types of catecholamines are dopamine, norepin...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Treatment
There is no cure for MSA. There is no known way to prevent the disease from getting worse. The goal of treatment is to control symptoms.
Dopaminergic medicines, such as levodopa and carbidopa, may be used to reduce early or mild tremors.
But, for many people with MSA these medicines do not work well.
Medicines may be used to treat low blood pressure.
A pacemaker that is programmed to stimulate the heart to beat at a rapid rate (faster than 100 beats per minute) may increase blood pressure for some people.
Constipation can be treated with a high-fiber diet and laxatives. Medicines are available to treat erection problems.
Outlook (Prognosis)
Outcome for MSA is poor. Loss of mental and physical functions slowly get worse. Early death is likely. People typically live 7 to 9 years after diagnosis.
When to Contact a Medical Professional
Call your provider if you develop symptoms of this disorder.
Call your provider if you have been diagnosed with MSA and your symptoms return or get worse. Also call if new symptoms appear, including possible side effects of medicines, such as:
- Changes in alertness/behavior/mood
- Delusional behavior
- Dizziness
-
Hallucinations
Hallucinations
Hallucinations involve sensing things such as visions, sounds, or smells that seem real but are not. These things are created by the mind.
Read Article Now Book Mark Article - Involuntary movements
- Loss of mental functioning
- Nausea or vomiting
- Severe confusion or disorientation
If you have a family member with MSA and their condition declines to the point that you are unable to care for the person at home, seek advice from your family member's provider.
References
Fanciulli A, Wenning GK. Multiple system atrophy. N Engl J Med . 2015;372(3):249-263. PMID: 25587949 www.ncbi.nlm.nih.gov/pubmed/25587949 .
Jankovic J. Parkinson disease and other movement disorders. In: Daroff RB, Jankovic J, Mazziotta JC, Pomeroy SL, eds. Bradley's Neurology in Clinical Practice . 7th ed. Philadelphia, PA: Elsevier; 2016:chap 96.
-
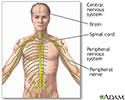
Central nervous system - illustration
The central nervous system is comprised of the brain and spinal cord. The peripheral nervous system includes all peripheral nerves.
Central nervous system
illustration
Review Date: 10/24/2016
Reviewed By: Amit M. Shelat, DO, FACP, Attending Neurologist and Assistant Professor of Clinical Neurology, SUNY Stony Brook, School of Medicine, Stony Brook, NY. Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.