Limb-girdle muscular dystrophies
Muscular dystrophy - limb-girdle type (LGMD)
Limb-girdle muscular dystrophies include at least 18 different inherited disorders. (There are 16 known genetic forms.) These disorders first affect the muscles around the shoulder girdle and hips. These diseases get worse. Eventually, it may involve other muscles.
Causes
Limb-girdle muscular dystrophies are a large group of genetic diseases in which there is muscle weakness and wasting (muscular dystrophy).
In most cases, both parents must pass on the non-working (defective) gene for a child to have the disease (autosomal recessive inheritance). In some rare types, only one parent needs to pass on the non-working gene to affect the child. This is called autosomal dominant inheritance. For 16 of these conditions, the defective gene has been discovered. For others, the gene is not yet known.
An important risk factor is having a family member with muscular dystrophy .
Muscular dystrophy
Muscular dystrophy is a group of inherited disorders that cause muscle weakness and loss of muscle tissue, which get worse over time.

Symptoms
Most often, the first sign is pelvic muscle weakness. Examples of this include trouble standing from a sitting position without using the arms, or difficulty climbing stairs. The weakness starts in childhood to young adulthood.
Other symptoms include:
- Abnormal, sometimes waddling, walk
- Joints that are fixed in a contracted position (late in the disease)
- Large and muscular-looking calves (pseudohypertrophy), which are not actually strong
- Loss of muscle mass, thinning of certain body parts
- Low back pain
-
Palpitations
or passing-out spells
Palpitations
Palpitations are feelings or sensations that your heart is pounding or racing. They can be felt in your chest, throat, or neck. You may:Have an unpl...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Shoulder weakness
- Weakness of the muscles in the face (later in the disease)
- Weakness in the muscles of the lower legs, feet, lower arms, and hands (later in the disease)
Exams and Tests
Tests may include:
-
Blood creatine kinase levels
Blood creatine kinase levels
Creatine phosphokinase (CPK) is an enzyme in the body. It is found mainly in the heart, brain, and skeletal muscle. This article discusses the test...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - DNA testing
-
Echocardiogram
or
ECG
Echocardiogram
An echocardiogram is a test that uses sound waves to create pictures of the heart. The picture and information it produces is more detailed than a s...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleECG
An electrocardiogram (ECG) is a test that records the electrical activity of the heart.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Electromyogram
(EMG) testing
Electromyogram
Electromyography (EMG) is a test that checks the health of the muscles and the nerves that control the muscles.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Muscle biopsy
Muscle biopsy
A muscle biopsy is the removal of a small piece of muscle tissue for examination.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Treatment
There are no known treatments that reverse the muscle weakness. Gene therapy may become available in the future. Supportive treatment can decrease the complications of the disease.
The condition is managed based on the person’s symptoms. It includes:
- Heart monitoring
- Mobility aids
- Physical therapy
- Respiratory care
- Weight control
Surgery is sometimes needed for any bone or joint problems.
Support Groups
The Muscular Dystrophy Association is an excellent resource (800-572-1717).
Outlook (Prognosis)
In general, people tend to have weakness that slowly gets worse in affected muscles and spreads.
The disease causes loss of movement. The person may be dependent on a wheelchair within 20 to 30 years.
Heart muscle weakness and abnormal electrical activity of the heart can increase the risk of palpitations, fainting, and sudden death. Most people with this group of diseases live into adulthood, but do not reach their full life expectancy.
Possible Complications
People with limb-girdle muscular dystrophies may experience complications such as:
- Abnormal heart rhythms
- Contractures of the joints
- Difficulties with activities of daily living due to shoulder weakness
- Progressive weakness, which may lead to needing a wheelchair
When to Contact a Medical Professional
Call your health care provider if you or your child feels weak while rising from a squatting position. Call a geneticist if you or a family member has been diagnosed with muscular dystrophy and you are planning a pregnancy.
Prevention
Genetic counseling may help some couples and families learn about the risks and help with family planning.
Some of the complications can be prevented with appropriate treatment. For example, a cardiac pacemaker or defibrillator can greatly reduce the risk of sudden death due to an abnormal heart rhythm. Physical therapy may be able to prevent or delay contractures and improve quality of life.
Affected people may want to do DNA banking. DNA testing is recommended for those who are affected. This helps to identify the family gene mutation. Once the mutation is found, prenatal DNA testing, testing for carriers, and pre-implantation genetic diagnosis are possible.
References
Mohassel P, Bonnemann CG. Limb-girdle muscular dystrophies. In: Darras BT, Jones R, Ruan MM, DeVivo DC, eds.
Neuromuscular Disorders Of Infancy, Childhood, And Adolescence
. 2nd ed. London, UK: Elsevier; 2015:chap 34.
Sarnat HB. Limb-girdle muscular dystrophies. In: Kliegman RM, Stanton BF, St Geme JW, Schor N, eds. Nelson Textbook of Pediatrics . 20th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 609.
-
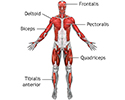
Superficial anterior muscles - illustration
Superficial muscles are close to the surface of the skin. Muscles which lie closer to bone or internal organs are called deep muscles.
Superficial anterior muscles
illustration
Review Date: 10/27/2015
Reviewed By: Chad Haldeman-Englert, MD, FACMG, Fullerton Genetics Center, Asheville, NC. Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.