Membranoproliferative glomerulonephritis
Membranoproliferative GN I; Membranoproliferative GN II; Mesangiocapillary glomerulonephritis; Membranoproliferative glomerulonephritis; Lobular GN; Glomerulonephritis - membranoproliferative; MPGN type I; MPGN type II
Membranoproliferative glomerulonephritis is a kidney disorder that involves inflammation and changes to kidney cells. It may lead to kidney failure .
Kidney failure
Chronic kidney disease is the slow loss of kidney function over time. The main job of the kidneys is to remove wastes and excess water from the body...

Causes
Glomerulonephritis is an inflammation of the glomeruli. The glomeruli of the kidney help filter wastes and fluids from the blood to form urine.
Glomerulonephritis
Glomerulonephritis is a type of kidney disease in which the part of your kidneys that helps filter waste and fluids from the blood is damaged....

Membranoproliferative glomerulonephritis (MPGN) is a form of glomerulonephritis caused by an abnormal immune response . Deposits of antibodies build up in a part of the kidneys called the glomerular basement membrane. This membrane helps filter wastes and extra fluids from the blood.
Immune response
The immune response is how your body recognizes and defends itself against bacteria, viruses, and substances that appear foreign and harmful....

Antibodies
An antibody is a protein produced by the body's immune system when it detects harmful substances, called antigens. Examples of antigens include micr...

Damage to this membrane affects the kidney's ability to create urine normally. It may allow blood and protein to leak into the urine. If enough protein leaks into the urine, fluid may leak out of the blood vessels into body tissues, leading to swelling ( edema ). Nitrogen waste products may also build up in the blood ( azotemia ).
Edema
Swelling is the enlargement of organs, skin, or other body parts. It is caused by a buildup of fluid in the tissues. The extra fluid can lead to a ...

Azotemia
Prerenal azotemia is an abnormally high level of nitrogen waste products in the blood.

The 2 forms of this disease are MPGN I and MPGN II.
Most people with the disease have type I. MPGN II is much less common. It also tends to get worse faster than MPGN I.
Causes of MPGN may include:
-
Autoimmune diseases (
systemic lupus erythematosus
,
scleroderma
,
Sjögren syndrome
,
sarcoidosis
Systemic lupus erythematosus
Systemic lupus erythematosus (SLE) is an autoimmune disease. In this disease, the body's immune system mistakenly attacks healthy tissue. It can af...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleScleroderma
Scleroderma is a disease that involves the buildup of scar-like tissue in the skin and elsewhere in the body. It also damages the cells that line th...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleSjögren syndrome
Sjögren syndrome is an autoimmune disorder in which the glands that produce tears and saliva are destroyed. This causes dry mouth and dry eyes. The...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleSarcoidosis
Sarcoidosis is a disease in which inflammation occurs in the lymph nodes, lungs, liver, eyes, skin, or other tissues.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Cancer (leukemia, lymphoma)
-
Infections (
hepatitis B
,
hepatitis C
,
endocarditis
,
malaria
)
Hepatitis B
Hepatitis B is irritation and swelling (inflammation) of the liver due to infection with the hepatitis B virus (HBV). Other types of viral hepatitis ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleHepatitis C
Hepatitis C is a viral disease that leads to swelling (inflammation) of the liver. Other types of viral hepatitis include:Hepatitis AHepatitis BHepat...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleEndocarditis
Endocarditis is inflammation of the inside lining of the heart chambers and heart valves (endocardium). It is caused by a bacterial or, rarely a fun...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleMalaria
Malaria is a parasitic disease that involves high fevers, shaking chills, flu-like symptoms, and anemia.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Symptoms
Symptoms may include any of the following:
-
Blood in the urine
Blood in the urine
Blood in your urine is called hematuria. The amount may be very small and only detected with urine tests or under a microscope. In other cases, the...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Changes in mental status
such as
decreased alertness
or decreased concentration
Changes in mental status
Confusion is the inability to think as clearly or quickly as you normally do. You may feel disoriented and have difficulty paying attention, remembe...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleDecreased alertness
Decreased alertness is a state of reduced awareness. A coma is a state of decreased alertness from which a person cannot be awakened. A long-term co...
Read Article Now Book Mark Article -
Cloudy urine
Cloudy urine
Blood in your urine is called hematuria. The amount may be very small and only detected with urine tests or under a microscope. In other cases, the...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Dark urine
(smoke, cola, or tea colored)
Dark urine
Blood in your urine is called hematuria. The amount may be very small and only detected with urine tests or under a microscope. In other cases, the...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Decrease in urine volume
Decrease in urine volume
Decreased urine output means that you produce less urine than normal. Most adults make at least 500 ml of urine in 24 hours (a little over 2 cups)....
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Foamy urine
-
Swelling
of any part of the body
Swelling
Swelling is the enlargement of organs, skin, or other body parts. It is caused by a buildup of fluid in the tissues. The extra fluid can lead to a ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Exams and Tests
The health care provider will examine you and ask about your symptoms. The provider may find that you have signs of too much fluid in the body, such as:
- Swelling, often in the legs
- Abnormal sounds when listening to your heart and lungs with a stethoscope
- You may have high blood pressure
The following tests help confirm the diagnosis:
-
BUN
and
creatinine
blood test
BUN
BUN stands for blood urea nitrogen. Urea nitrogen is what forms when protein breaks down. A test can be done to measure the amount of urea nitrogen ...
Read Article Now Book Mark ArticleCreatinine
The creatinine blood test measures the level of creatinine in the blood. This test is done to see how well your kidneys are working. Creatinine can ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Blood complement levels
Blood complement levels
Complement is a blood test that measures the activity of certain proteins in the liquid portion of your blood. The complement system is a group of pr...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Urinalysis
Urinalysis
Urinalysis is the physical, chemical, and microscopic examination of urine. It involves a number of tests to detect and measure various compounds th...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Urine protein
Urine protein
The protein urine dipstick test measures the presence of proteins, such as albumin, in a urine sample. Albumin and protein can also be measured using...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
kidney biopsy
(to confirm membranoproliferative GN I or II)
Kidney biopsy
A kidney biopsy is the removal of a small piece of kidney tissue for examination.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Treatment
Treatment depends on the symptoms. The goals of treatment are to reduce symptoms, prevent complications, and slow the progression of the disorder.
You may need a change in diet. This may include limiting salt, fluids, or protein to help control high blood pressure, swelling, and the buildup of waste products in the blood.
Medicines that may be prescribed include:
- Blood pressure medicines
- Dipyridamole, with or without aspirin
- Diuretics
- Medicines to suppress the immune system, such as cyclophosphamide
- Steroids
Treatment is more effective in children than in adults. Dialysis or kidney transplant may eventually be needed to manage kidney failure.
Kidney transplant
A kidney transplant is surgery to place a healthy kidney into a person with kidney failure.

Outlook (Prognosis)
The disorder often slowly gets worse and eventually results in chronic kidney failure .
Chronic kidney failure
Chronic kidney disease is the slow loss of kidney function over time. The main job of the kidneys is to remove wastes and excess water from the body...

Half of people with this condition develop chronic kidney failure within 10 years. This is more likely in those who have higher levels of protein in their urine.
Possible Complications
Complications that may result from this disease include:
-
Acute nephritic syndrome
Acute nephritic syndrome
Acute nephritic syndrome is a group of symptoms that occur with some disorders that cause swelling and inflammation of the glomeruli in the kidney, o...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Acute renal failure
Acute renal failure
Acute kidney failure is the rapid (less than 2 days) loss of your kidneys' ability to remove waste and help balance fluids and electrolytes in your b...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Chronic kidney disease
Chronic kidney disease
Chronic kidney disease is the slow loss of kidney function over time. The main job of the kidneys is to remove wastes and excess water from the body...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
When to Contact a Medical Professional
Call for an appointment with your provider if:
- You have symptoms of this condition
- Your symptoms get worse or do not go away
- You develop new symptoms, including decreased urine output
Prevention
Preventing infections such as hepatitis or managing diseases such as lupus may help prevent MPGN.
References
Schena FP, Alpers CE. Membranoproliferative glomerulonephritis and cryoglobulinemic glomerulonephritis. In: Johnson RJ, Feehally J, Floege J, eds. Comprehensive Clinical Nephrology . 5th ed. Philadelphia, PA: Elsevier Saunders; 2015:chap 21.
-
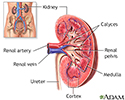
Kidney anatomy - illustration
The kidneys are responsible for removing wastes from the body, regulating electrolyte balance and blood pressure, and stimulating red blood cell production.
Kidney anatomy
illustration
Review Date: 9/22/2015
Reviewed By: Charles Silberberg, DO, private practice specializing in nephrology, affiliated with New York Medical College, Division of Nephrology, Valhalla, NY. Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.