Cervical spondylosis
Cervical osteoarthritis; Arthritis - neck; Neck arthritis; Chronic neck pain; Degenerative disk disease
Cervical spondylosis is a disorder in which there is wear on the cartilage (disks) and bones of the neck (cervical vertebrae). It is a common cause of chronic neck pain.
Causes
Cervical spondylosis is caused by aging and chronic wear on the cervical spine. This includes the disks or cushions between the neck vertebrae and the joints between the bones of the cervical spine. There may be abnormal growths or spurs on the bones of the spine (vertebrae).
Chronic
Chronic refers to something that continues over an extended period of time. A chronic condition is usually long-lasting and does not easily or quick...

Over time, these changes can press down on (compress) one or more of the nerve roots. In advanced cases, the spinal cord becomes involved. This can affect not just the arms, but the legs as well.
Everyday wear and tear may start these changes. People who are very active at work or in sports may be more likely to have them.
The major risk factor is aging. By age 60, most people show signs of cervical spondylosis on x-ray. Other factors that can make someone more likely to develop spondylosis are:
- Being overweight and not exercising
- Having a job that requires heavy lifting or a lot of bending and twisting
- Past neck injury (often several years before)
- Past spine surgery
-
Ruptured or slipped disk
Ruptured or slipped disk
A herniated (slipped) disk occurs when all or part of a disk is forced through a weakened part of the disk. This may place pressure on nearby nerves...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Severe arthritis
-
Small fractures to the spine from osteoporosis
Small fractures to the spine from osteo...
Compression fractures of the back are broken vertebrae. Vertebrae are the bones of the spine.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Symptoms
Symptoms often develop slowly over time. But they may start or get worse suddenly. The pain may be mild, or it can be deep and so severe that you are unable to move.
You may feel the pain over the shoulder blade. It may spread to the upper arm, forearm, or fingers (in rare cases).
The pain may get worse:
- After standing or sitting
- At night
- When you sneeze, cough, or laugh
- When you bend the neck backwards or walk more than a few yards or more than a few meters
You may also have weakness in certain muscles. Sometimes, you may not notice it until your doctor examines you. In other cases, you will notice that you have a hard time lifting your arm, squeezing tightly with one of your hands, or other problems.
Other common symptoms are:
- Neck stiffness that gets worse over time
-
Numbness or
abnormal sensations
in the shoulders or arms
Abnormal sensations
Numbness and tingling are abnormal sensations that can occur anywhere in your body, but they are often felt in your fingers, hands, feet, arms, or le...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Headaches
, especially in the back of the head
Headaches
A headache is pain or discomfort in the head, scalp, or neck. Serious causes of headaches are rare. Most people with headaches can feel much better...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Less common symptoms are:
-
Loss of balance
Loss of balance
Dizziness is a term that is often used to describe 2 different symptoms: lightheadedness and vertigo. Lightheadedness is a feeling that you might fai...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Pain or numbness in the legs
- Loss of control over the bladder or bowels (if there is pressure on the spinal cord)
Exams and Tests
A physical exam may show that you have trouble moving your head toward your shoulder and rotating your head.
Your health care provider may ask you to bend your head forward and to each side while putting slight downward pressure on the top of your head. Increased pain or numbness during this test is usually a sign that there is pressure on a nerve in your spine.
Weakness or loss of feeling can be signs of damage to certain nerve roots or to the spinal cord.
A spine or neck x-ray may be done to look for arthritis or other changes in your spine.
Neck x-ray
A neck x-ray is an imaging test to look at cervical vertebrae. These are the 7 bones of the spine in the neck.

MRI of the neck is done when you have:
MRI of the neck
A cervical MRI (magnetic resonance imaging) scan uses energy from strong magnets to create pictures of the part of the spine that runs through the ne...
- Severe neck or arm pain that does not get better with treatment
- Weakness or numbness in your arms or hands
EMG and nerve conduction velocity test may be done to examine nerve root function.
EMG
Electromyography (EMG) is a test that checks the health of the muscles and the nerves that control the muscles.

Nerve conduction velocity
Nerve conduction velocity (NCV) is a test to see how fast electrical signals move through a nerve.

Treatment
Your doctor and other health professionals can help you manage your pain so that you can stay active.
- Your doctor may refer you for physical therapy. The physical therapist will help you reduce your pain using stretches. The therapist will teach you exercises that make your neck muscles stronger.
-
The therapist can also use
neck traction
to relieve some of the pressure in your neck.
Neck traction
Traction means pulling on part of the body. Most often, traction uses devices such as weights and pulleys to put tension on a displaced bone or joint...
Read Article Now Book Mark Article - You may also see a massage therapist, someone who performs acupuncture, or someone who does spinal manipulation (a chiropractor, osteopathic doctor, or physical therapist). Sometimes, a few visits will help with neck pain.
- Cold packs and heat therapy may help your pain during flare-ups.
A type of talk therapy called cognitive behavioral therapy may be helpful if the pain is having a serious impact on your life. This technique helps you better understand your pain and teaches you how to manage it.
Medicines can help your neck pain. Your doctor may prescribe nonsteroidal anti-inflammatory medicines (NSAIDs) for long-term pain control. Opioids may be prescribed if the pain is severe and does not respond to NSAIDs.
If the pain does not respond to these treatments, or you have a loss of movement or feeling, surgery is considered. Surgery is done to relieve the pressure on the nerves or spinal cord.
Outlook (Prognosis)
Most people with cervical spondylosis have some long-term symptoms. These symptoms improve with non-surgical treatment and do not need surgery.
Many people with this problem are able to maintain an active life. Some people will have to live with chronic (long-term) pain.
Possible Complications
This condition may lead to the following:
-
Inability to hold in feces (
fecal incontinence
) or urine (
urinary incontinence
)
Fecal incontinence
Bowel incontinence is the loss of bowel control, causing you to pass stool unexpectedly. This can range from sometimes leaking a small amount of sto...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleUrinary incontinence
Urinary (or bladder) incontinence happens when you are not able to keep urine from leaking out of your urethra. The urethra is the tube that carries...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Loss of muscle function or feeling
- Permanent disability (occasionally)
- Poor balance
When to Contact a Medical Professional
Call your provider if:
- The condition becomes worse
- There are signs of complications
-
You develop new symptoms (such as
loss of movement
or feeling in an area of the body)
Loss of movement
Muscle function loss is when a muscle does not work or move normally. The medical term for complete loss of muscle function is paralysis.
Read Article Now Book Mark Article - You lose control of your bladder or bowels (call right away)
References
Fast A, Dudkiewicz I. Cervical degenerative disease. In: Frontera WR, Silver JK, Rizzo TD Jr, eds. Essentials of Physical Medicine and Rehabilitation . 3rd ed. Philadelphia, PA: Elsevier Saunders; 2015:chap 3.
Kshettry VR. Cervical spondylosis. In: Benzel EC, ed. Spine Surgery . 3rd ed. Philadelphia, PA: Elsevier Saunders; 2012:chap 82.
Takagi I, Eliyas K, Stadlan N. Cervical spondylosis: an update on pathophysiology, clinical manifestation, and management strategies. Dis Mon . 2011;57:583-91. PMID: 22036114 www.ncbi.nlm.nih.gov/pubmed/22036114 .
-
Skeletal spine - illustration
The spine is divided into several sections. The cervical vertebrae make up the neck. The thoracic vertebrae comprise the chest section and have ribs attached. The lumbar vertebrae are the remaining vertebrae below the last thoracic bone and the top of the sacrum. The sacral vertebrae are caged within the bones of the pelvis, and the coccyx represents the terminal vertebrae or vestigial tail.
Skeletal spine
illustration
-
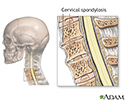
Cervical spondylosis - illustration
Cervical spondylosis is a disorder that results from abnormal growth of the bones of the neck and degeneration and mineral deposits in the cushions between the vertebrae. Progressive neck pain is a key indication of cervical spondylosis. It may be the only symptom in many cases. Examination often shows limited ability to bend the head toward the shoulders and limited ability to rotate the head. The goal of treatment is relief of pain and prevention of permanent spinal cord and nerve root injury.
Cervical spondylosis
illustration
-
Skeletal spine - illustration
The spine is divided into several sections. The cervical vertebrae make up the neck. The thoracic vertebrae comprise the chest section and have ribs attached. The lumbar vertebrae are the remaining vertebrae below the last thoracic bone and the top of the sacrum. The sacral vertebrae are caged within the bones of the pelvis, and the coccyx represents the terminal vertebrae or vestigial tail.
Skeletal spine
illustration
-
Cervical spondylosis - illustration
Cervical spondylosis is a disorder that results from abnormal growth of the bones of the neck and degeneration and mineral deposits in the cushions between the vertebrae. Progressive neck pain is a key indication of cervical spondylosis. It may be the only symptom in many cases. Examination often shows limited ability to bend the head toward the shoulders and limited ability to rotate the head. The goal of treatment is relief of pain and prevention of permanent spinal cord and nerve root injury.
Cervical spondylosis
illustration
Review Date: 4/13/2015
Reviewed By: Dennis Ogiela, MD, Orthopedic Surgery and Physical Medicine and Rehabilitation, Danbury Hospital, Danbury, CT. Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.