Amebiasis
Amebic dysentery; Intestinal amebiasis; Amebic colitis; Diarrhea - amebiasis
Amebiasis is an infection of the intestines. It is caused by the parasite Entamoeba histolytica .
Causes
E. histolytica can live in the large intestine (colon) without causing damage to the intestine. In some cases, it invades the colon wall, causing colitis , acute dysentery, or long-term (chronic) diarrhea. The infection can also spread through the bloodstream to the liver. In rare cases, it can spread to the lungs, brain, or other organs.
Colitis
Colitis is swelling (inflammation) of the large intestine (colon).

This condition occurs worldwide. It is most common in tropical areas that have crowded living conditions and poor sanitation. Africa, Mexico, parts of South America, and India have major health problems due to this condition.
The parasite may spread:
- Through food or water contaminated with stools
- Through fertilizer made of human waste
- From person to person, particularly by contact with the mouth or rectal area of an infected person
Risk factors for severe amebiasis include:
- Alcohol use
- Cancer
- Malnutrition
- Older or younger age
- Pregnancy
- Recent travel to a tropical region
- Use of corticosteroid medicine to suppress the immune system
In the United States, amebiasis is most common among those who live in institutions or people who have traveled to an area where amebiasis is common.
Symptoms
Most people with this infection do not have symptoms. If symptoms occur, they are seen 7 to 28 days after being exposed to the parasite.
Mild symptoms may include:
- Abdominal cramps
- Diarrhea: passage of 3 to 8 semiformed stools per day, or passage of soft stools with mucus and occasional blood
- Fatigue
- Excessive gas
-
Rectal pain while having a bowel movement (
tenesmus
)
Tenesmus
Tenesmus is the feeling that you need to pass stools, even though your bowels are already empty. It may involve straining, pain, and cramping....
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Unintentional weight loss
Unintentional weight loss
Unexplained weight loss is a decrease in body weight, when you did not try to lose the weight on your own. Many people gain and lose weight. Uninten...
Read Article Now Book Mark Article
Severe symptoms may include:
- Abdominal tenderness
-
Bloody stools
, including passage of liquid stools with streaks of blood, passage of 10 to 20 stools per day
Bloody stools
Bloody stools often are a sign of a problem in the digestive tract. Blood in the stool may come from anywhere along your digestive tract from your m...
Read Article Now Book Mark Article - Fever
- Vomiting
Exams and Tests
The health care provider will perform a physical exam. You will be asked about your medical history, especially if you have recently traveled overseas.
Examination of the abdomen may show liver enlargement or tenderness in the abdomen.
Liver enlargement
Hepatomegaly is swelling of the liver beyond its normal size. If both the liver and spleen are enlarged, it is called hepatosplenomegaly.

Tests that may be ordered include:
- Blood test for amebiasis
-
Examination of the inside of the lower large bowel (
sigmoidoscopy
)
Sigmoidoscopy
Sigmoidoscopy is a procedure used to see inside the sigmoid colon and rectum. The sigmoid colon is the area of the large intestine nearest to the re...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Stool test
-
Microscope examination of stool samples
, usually with multiple samples over several days
Microscope examination of stool samples
Stool ova and parasites exam is a lab test to look for parasites or eggs (ova) in a stool sample. The parasites are associated with intestinal infec...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Treatment
Treatment depends on how severe the infection is. Usually, antibiotics are prescribed.
If you are vomiting, you may be given medicines through a vein ( intravenously ) until you can take them by mouth. Medicines to stop diarrhea are usually not prescribed, because they can make the condition worse.
Intravenously
Intravenous means "within a vein. " Most often it refers to giving medicines or fluids through a needle or tube inserted into a vein. This allows th...
After antibiotic treatment, your stool will likely be rechecked to make sure the infection has been cleared.
Outlook (Prognosis)
Outcome is usually good with treatment. Usually, the illness lasts about 2 weeks, but it can come back if you do not get treated.
Possible Complications
Complications of amebiasis may include:
-
Liver abscess
Liver abscess
Amebic liver abscess is a collection of pus in the liver in response to an intestinal parasite called Entamoeba histolytica.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Medicine side effects, including nausea
- Spread of the parasite through the blood to the liver, lungs, brain, or other organs
When to Contact a Medical Professional
Call your health care provider if you have diarrhea that does not go away or gets worse.
Prevention
When traveling in countries where sanitation is poor, drink purified or boiled water. Do not eat uncooked vegetables or unpeeled fruit.
References
Petri WA, Haque R. Entamoeba species, including amebic colitis and liver abscess. In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases, Updated Edition . 8th ed. Philadelphia, PA: Elsevier Saunders; 2015:chap 274.
Petri WA, Lima AAM. Amebiasis. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine . 25th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 352.
-
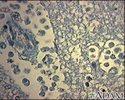
Amebic brain abscess - illustration
Amebiasis, normally an infection of the intestinal tract, may spread and infect other organs such as the liver or brain. Infection of the brain can be fatal. In this slide, ameba are shown in a sample of brain tissue. Ameba represent a serious infection in immunocompromised individuals. (Image courtesy of the Centers for Disease Control and Prevention.)
Amebic brain abscess
illustration
-
Digestive system - illustration
The esophagus, stomach, large and small intestine, aided by the liver, gallbladder and pancreas convert the nutritive components of food into energy and break down the non-nutritive components into waste to be excreted.
Digestive system
illustration
-
Digestive system organs - illustration
The digestive system organs in the abdominal cavity include the liver, gallbladder, stomach, small intestine and large intestine.
Digestive system organs
illustration
-
Amebic brain abscess - illustration
Amebiasis, normally an infection of the intestinal tract, may spread and infect other organs such as the liver or brain. Infection of the brain can be fatal. In this slide, ameba are shown in a sample of brain tissue. Ameba represent a serious infection in immunocompromised individuals. (Image courtesy of the Centers for Disease Control and Prevention.)
Amebic brain abscess
illustration
-
Digestive system - illustration
The esophagus, stomach, large and small intestine, aided by the liver, gallbladder and pancreas convert the nutritive components of food into energy and break down the non-nutritive components into waste to be excreted.
Digestive system
illustration
-
Digestive system organs - illustration
The digestive system organs in the abdominal cavity include the liver, gallbladder, stomach, small intestine and large intestine.
Digestive system organs
illustration
Review Date: 7/31/2016
Reviewed By: Jatin M. Vyas, MD, PhD, Assistant Professor in Medicine, Harvard Medical School; Assistant in Medicine, Division of Infectious Disease, Department of Medicine, Massachusetts General Hospital, Boston, MA. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.