Coarctation of the aorta
Aortic coarctation
The aorta carries blood from the heart to the vessels that supply the body with blood. If part of the aorta is narrowed, it is hard for blood to pass through the artery. This is called coarctation of the aorta. It is a type of birth defect.
Causes
The exact cause of coarctation of the aorta is unknown. It results from abnormalities in development of the aorta prior to birth.
Aortic coarctation is more common in persons with certain genetic disorders, such as Turner syndrome .
Turner syndrome
Turner syndrome is a rare genetic condition in which a female does not have the usual pair of 2 X chromosomes.
Aortic coarctation is one of the more common heart conditions that are present at birth (congenital heart defects). It is most often diagnosed in children or adults under age 40.
People who have this problem with their aorta may also have a weak area in the wall of blood vessels in their brain. This weakness causes the blood vessel to bulge or balloon out. They can increase the risk for stroke.
Coarctation of the aorta may be seen with other congenital heart defects, such as:
- Bicuspid aortic valve
- Defects in which only one ventricle is present
- Ventricular septal defect
Symptoms
Symptoms depend on how much blood can flow through the artery. Other heart defects may also play a role.
About half of newborns with this problem will have symptoms in the first few days of life. These can include breathing fast, problems eating, increased irritability, and increased sleepiness or becoming poorly responsive.
In milder cases, symptoms may not develop until the child has reached adolescence. Symptoms include:
- Chest pain
- Cold feet or legs
-
Dizziness
or
fainting
Dizziness
Dizziness is a term that is often used to describe 2 different symptoms: lightheadedness and vertigo. Lightheadedness is a feeling that you might fai...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleFainting
Fainting is a brief loss of consciousness due to a drop in blood flow to the brain. The episode most often lasts less than a couple of minutes and y...
Read Article Now Book Mark Article - Decreased ability to exercise
- Failure to thrive
-
Leg cramps
with exercise
Leg cramps
Muscle cramps are when a muscle gets tight (contracts) without you trying to tighten it, and it does not relax. Cramps may involve all or part of on...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Nosebleed
Nosebleed
A nosebleed is loss of blood from the tissue lining the nose. Bleeding most often occurs in 1 nostril only.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Poor growth
- Pounding headache
- Shortness of breath
There may also be no symptoms.
Exams and Tests
The health care provider will perform a physical exam and check the blood pressure and pulse in the arms and legs.
- The pulse in the groin (femoral) area or feet will be weaker than the pulse in the arms or neck (carotid). Sometimes, the femoral pulse may not be felt at all.
- The blood pressure in the legs is usually weaker than in the arms. Blood pressure is usually higher in the arms after infancy.
The provider will use a stethoscope to listen to the heart and check for murmurs. People with aortic coarctation often have a harsh-sounding murmur that can be heard from the back. Other types of murmurs may also be present.
Coarctation is often discovered during a newborn's first exam or a well-baby exam. Taking the pulse in an infant is an important part of the examination because there may not be any other symptoms until the child is older.
Tests to diagnose this condition may include:
-
Cardiac catheterization
and aortography
Cardiac catheterization
Cardiac catheterization involves passing a thin flexible tube (catheter) into the right or left side of the heart. The catheter is most often insert...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Chest x-ray
Chest x-ray
A chest x-ray is an x-ray of the chest, lungs, heart, large arteries, ribs, and diaphragm.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Echocardiography
is the most common test to diagnose this condition, and it may also be used to monitor the person after surgery
Echocardiography
An echocardiogram is a test that uses sound waves to create pictures of the heart. The picture and information it produces is more detailed than a s...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Heart CT
may be needed in older children
Heart CT
A computed tomography (CT) scan of the heart is an imaging method that uses x-rays to create detailed pictures of the heart and its blood vessels. Th...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
MRI
or
MR angiography
of the chest may be needed in older children
MRI
A magnetic resonance imaging (MRI) scan is an imaging test that uses powerful magnets and radio waves to create pictures of the body. It does not us...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleMR angiography
Magnetic resonance angiography (MRA) is an MRI exam of the blood vessels. Unlike traditional angiography that involves placing a tube (catheter) int...
Read Article Now Book Mark Article
Both Doppler ultrasound and cardiac catheterization can be used to see if there are any differences in blood pressure in different areas of the aorta.
Treatment
Most newborns with symptoms will have surgery either right after birth or soon afterward. They will first receive medicines to stabilize them.
Children who are diagnosed when they are older will also need surgery. In most cases, the symptoms are not as severe, so more time can be taken to plan for surgery.
During surgery, the narrowed part of the aorta will be removed or opened.
-
If the problem area is small, the two free ends of the aorta may be re-connected. This is called an end-to-end
anastomosis
.
Anastomosis
An anastomosis is a surgical connection between two structures. It usually means a connection that is created between tubular structures, such as bl...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
If a large part of the aorta is removed, a graft or one of the patient's own arteries may be used to fill the gap. The
graft
may be man-made or from a cadaver.
Graft
A Dacron graft is made out of a man-made (synthetic) polyester material. It is used to replace natural body tissues. Most Dacron grafts are in the ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Sometimes, doctors will try to stretch open the narrowed part of the aorta by using a balloon that is widened inside the blood vessel. This type of procedure is called a balloon angioplasty . It may be done instead of surgery, but it has a higher rate of failure.
Balloon angioplasty
The blood vessels that bring blood to your brain and face are called the carotid arteries. You have a carotid artery on each side of your neck. The...

Older children usually need medicines to treat high blood pressure after surgery. Some will need lifelong treatment for this problem.
Outlook (Prognosis)
Coarctation of the aorta can be cured with surgery. Symptoms quickly get better after surgery.
However, there is an increased risk for death due to heart problems among those who have had their aorta repaired. Lifelong follow-up with a cardiologist is encouraged.
Without treatment, most people die before age 40. For this reason, doctors most often recommend that the patient has surgery before age 10. Most of the time, surgery to fix the coarctation is done during infancy.
Narrowing or coarctation of the artery can return after surgery. This is more likely in persons who had surgery as a newborn.
Possible Complications
Complications that may occur before, during, or soon after surgery include:
-
An area of the aorta becomes very large or balloons out
An area of the aorta becomes very large...
The aorta is the main blood vessel that supplies blood to the abdomen, pelvis, and legs. An abdominal aortic aneurysm occurs when an area of the aor...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Tear in the wall of the aorta
Tear in the wall of the aorta
Aortic dissection is a serious condition in which there is a tear in the wall of the major artery carrying blood out of the heart (aorta). As the te...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Rupture of the aorta
- Bleeding in the brain
-
Early development of
coronary artery disease
(CAD)
Coronary artery disease
Stable angina is chest pain or discomfort that most often occurs with activity or emotional stress. Angina is due to poor blood flow through the blo...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Endocarditis
(infection in the heart)
Endocarditis
Endocarditis is inflammation of the inside lining of the heart chambers and heart valves (endocardium). It is caused by a bacterial or, rarely a fun...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Heart failure
Heart failure
Heart failure is a condition in which the heart is no longer able to pump oxygen-rich blood to the rest of the body efficiently. This causes symptom...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Hoarseness
- Kidney problems
- Paralysis of the lower half of the body (a rare complication of surgery to repair coarctation)
- Severe high blood pressure
-
Stroke
Stroke
A stroke occurs when blood flow to a part of the brain stops. A stroke is sometimes called a "brain attack. " If blood flow is cut off for longer th...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Long-term complications include:
- Continued or repeated narrowing of the aorta
- Endocarditis
- High blood pressure
When to Contact a Medical Professional
Call your provider if:
- You or your child has symptoms of coarctation of the aorta
-
You develop fainting or
chest pain
(these may be signs of a serious problem)
Chest pain
Chest pain is discomfort or pain that you feel anywhere along the front of your body between your neck and upper abdomen.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Prevention
There is no known way to prevent this disorder. However, being aware of your risk may lead to early diagnosis and treatment.
References
Fraser CD Jr, Carberry KE. Congenital heart disease. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery . 19th ed. Philadelphia, PA: Elsevier Saunders; 2012:chap 59.
Webb GD, Smallhorn JF, Therrien J, Redington AN. Congenital heart disease. In: Mann DL, Zipes DP, Libby P, Bonow RO, Braunwald E, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine . 10th ed. Philadelphia, PA: Elsevier Saunders; 2015:chap 62.
-
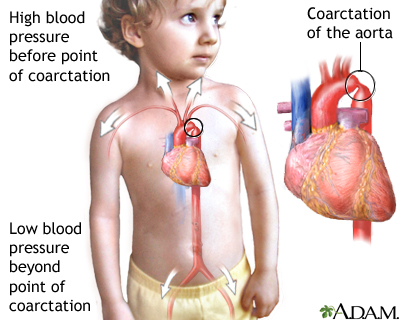
Coarctation of the aorta - illustration
Coarctation of the aorta is a birth defect in which the aorta, the major artery from the heart, is narrowed. The narrowing results in high blood pressure before the point of coarctation and low blood pressure beyond the point of coarctation. Most commonly, coarctation is located so that there is high blood pressure in the upper body and arms and low blood pressure in the lower body and legs. Symptoms can include localized hypertension, cold feet or legs, decreased exercise performance, and heart failure.
Coarctation of the aorta
illustration
-
Coarctation of the aorta - illustration
Coarctation of the aorta is a birth defect in which the aorta, the major artery from the heart, is narrowed. The narrowing results in high blood pressure before the point of coarctation and low blood pressure beyond the point of coarctation. Most commonly, coarctation is located so that there is high blood pressure in the upper body and arms and low blood pressure in the lower body and legs. Symptoms can include localized hypertension, cold feet or legs, decreased exercise performance, and heart failure.
Coarctation of the aorta
illustration
Review Date: 10/22/2015
Reviewed By: Larry A. Weinrauch MD, Assistant Professor of Medicine, Harvard Medical School, Cardiovascular Disease and Clinical Outcomes Research, Watertown, MA. Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.