Hemothorax
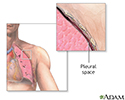
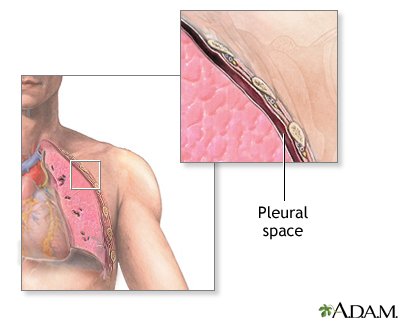
Hemothorax is a collection of blood in the space between the chest wall and the lung (the pleural cavity).
Causes
The most common cause of hemothorax is chest trauma. Hemothorax can also occur in people who have:
- Blood clotting defect
- Chest (thoracic) or heart surgery
- Death of lung tissue (pulmonary infarction)
-
Lung or pleural
cancer
-- primary or secondary (metastatic, or from another site)
Cancer
Cancer is the uncontrolled growth of abnormal cells in the body. Cancerous cells are also called malignant cells.
Read Article Now Book Mark Article - Tear in a blood vessel when placing a central venous catheter or when associated with severe high blood pressure
- Tuberculosis
Symptoms
Symptoms include:
-
Anxiety
Anxiety
Stress is a feeling of emotional or physical tension. It can come from any event or thought that makes you feel frustrated, angry, or nervous. Stres...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Chest pain
Chest pain
Chest pain is discomfort or pain that you feel anywhere along the front of your body between your neck and upper abdomen.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Low blood pressure
Low blood pressure
Low blood pressure occurs when blood pressure is much lower than normal. This means the heart, brain, and other parts of the body do not get enough ...
Read Article Now Book Mark Article - Pale, cool and clammy skin
-
Rapid heart rate
Rapid heart rate
A bounding pulse is a strong throbbing felt over one of the arteries in the body. It is due to a forceful heartbeat.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Rapid, shallow breathing
-
Restlessness
Restlessness
Agitation is an unpleasant state of extreme arousal. An agitated person may feel stirred up, excited, tense, confused, or irritable.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Shortness of breath
Shortness of breath
Breathing difficulty may involve:Difficult breathingUncomfortable breathingFeeling like you are not getting enough air
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Exams and Tests
Your health care provider may note decreased or absent breath sounds on the affected side. Signs or findings of hemothorax may be seen on the following tests:
-
Chest x-ray
Chest x-ray
A chest x-ray is an x-ray of the chest, lungs, heart, large arteries, ribs, and diaphragm.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
CT scan
CT scan
A computed tomography (CT) scan is an imaging method that uses x-rays to create pictures of cross-sections of the body. Related tests include:Abdomin...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Pleural fluid analysis
(often very bloody or blood-tinged)
Pleural fluid analysis
Pleural fluid analysis is a test that examines a sample of fluid that has collected in the pleural space. This is the space between the lining of th...
Read Article Now Book Mark Article -
Thoracentesis
(drainage of pleural fluid through a needle or catheter)
Thoracentesis
Thoracentesis is a procedure to remove fluid from the space between the lining of the outside of the lungs (pleura) and the wall of the chest....
Read Article Now Book Mark Article
Treatment
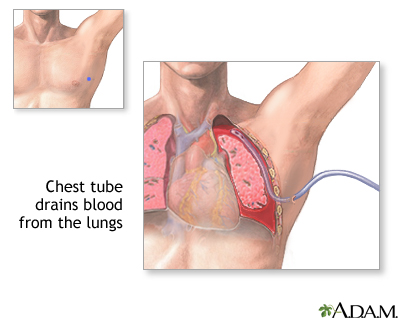
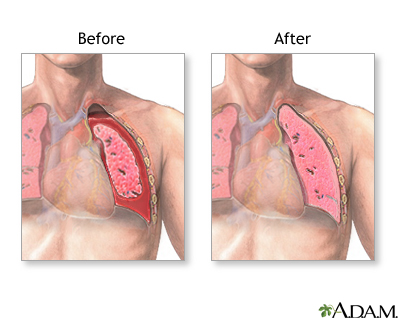
The goal of treatment is to get the person stable, stop the bleeding, and remove the blood and air in the pleural space.
- A chest tube is inserted through the chest wall between the ribs to drain the blood and air.
- It is left in place and attached to suction for several days to re-expand the lung.
If a chest tube alone does not control the bleeding, surgery ( thoracotomy ) may be needed to stop the bleeding.
Thoracotomy
Lung surgery is surgery done to repair or remove lung tissue. There are many common lung surgeries, including:Biopsy of an unknown growthLobectomy, ...

The cause of the hemothorax should be also treated. The underlying lung may have collapsed. This can lead to breathing difficulty. In people who have had an injury, chest tube drainage may be all that is needed. Surgery may not be necessary.
WHAT TO EXPECT AT THE EMERGENCY DEPARTMENT
The provider will measure and monitor the person's vital signs, including temperature, pulse, breathing rate, and blood pressure. Symptoms will be treated as needed. The person may receive:
- Breathing support. This may include oxygen, endotracheal intubation (tube through the nose or mouth into the trachea) and ventilator (breathing machine)
- Blood tests and possible blood transfusion
- Chest tube (tube through the skin and muscles between the ribs into the space around the lungs)) if there is lung collapse
- CAT/CT scan of the chest and abdomen
- EKG
- Fluids given through the vein
- Medicines to treat symptoms
-
X-rays of chest and abdomen or other parts of the body if there are additional injuries
Outlook (Prognosis)
The outcome depends on the cause of the hemothorax, the amount of blood loss and how quickly treatment is given.
In the case of major trauma, the outcome will depend on the severity of the injury and the rate of bleeding.
Possible Complications
Complications may include:
-
Collapsed lung
, or
pneumothorax
, leading to
respiratory
failure (inability to breathe properly, provide the body enough oxygen and remove carbon dioxide)
Collapsed lung
A collapsed lung occurs when air escapes from the lung. The air then fills the space outside of the lung, between the lung and chest wall. This bui...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticlePneumothorax
A collapsed lung occurs when air escapes from the lung. The air then fills the space outside of the lung, between the lung and chest wall. This bui...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleRespiratory
The words "respiratory" and "respiration" refer to the lungs and breathing.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Death
- Fibrosis or scarring of the pleural membranes and underlying lung tissue
-
Infection of the pleural fluid (
empyema
)
Empyema
Empyema is a collection of pus in the space between the lung and the inner surface of the chest wall (pleural space).
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Shock
and death in severe circumstances
Shock
Shock is a life-threatening condition that occurs when the body is not getting enough blood flow. Lack of blood flow means that the cells and organs...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
When to Contact a Medical Professional
Call 911 if you have:
- Any serious injury to the chest
- Chest pain or shortness of breath
Go to the emergency room or call the local emergency number (such as 911) if you have:
- Dizziness, lightheadedness, fever and cough, or a feeling of heaviness in your chest
- Severe chest, neck, jaw, shoulder or arm pain
-
Severe
difficulty breathing
Difficulty breathing
Breathing difficulty may involve:Difficult breathingUncomfortable breathingFeeling like you are not getting enough air
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Prevention
Use safety measures (such as seat belts) to avoid injury. Depending on the cause, a hemothorax may not be preventable.
References
Coimbra R, Hoyt DB. Chest wall trauma, hemothorax, and pneumothorax. In: Cameron JL, Cameron AM, eds. Current Surgical Therapy . 11th ed. Philadelphia, PA: Elsevier Saunders; 2014:1005-1009.
Eckstein M, Henderson SO. Thoracic trauma. In: Marx JA, Hockberger RS, Walls RM, et al, eds. Rosen's Emergency Medicine: Concepts and Clinical Practice . 8th ed. Philadelphia, PA: Elsevier Saunders; 2014:chap 45.
Light RW, Lee YCG. Pneumothorax, chylothorax, hemothorax, and fibrothorax. In: Broaddus VC, Mason RJ, Ernst JD, et al, eds. Murray & Nadel's Textbook of Respiratory Medicine . 6th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 81.
-
Aortic rupture, chest X-ray - illustration
Aortic rupture (a tear in the aorta, which is the major artery coming from the heart) can be seen on a chest x-ray. In this case, it was caused by a traumatic perforation of the thoracic aorta. This is how the x-ray appears when the chest is full of blood (right-sided hemothorax) seen here as cloudiness on the left side of the picture.
Aortic rupture, chest X-ray
illustration
-
Respiratory system - illustration
Air is breathed in through the nasal passageways, travels through the trachea and bronchi to the lungs.
Respiratory system
illustration
-
Chest tube insertion - series
Presentation
-
Aortic rupture, chest X-ray - illustration
Aortic rupture (a tear in the aorta, which is the major artery coming from the heart) can be seen on a chest x-ray. In this case, it was caused by a traumatic perforation of the thoracic aorta. This is how the x-ray appears when the chest is full of blood (right-sided hemothorax) seen here as cloudiness on the left side of the picture.
Aortic rupture, chest X-ray
illustration
-
Respiratory system - illustration
Air is breathed in through the nasal passageways, travels through the trachea and bronchi to the lungs.
Respiratory system
illustration
-
Chest tube insertion - series
Presentation
Review Date: 6/22/2016
Reviewed By: Jacob L. Heller, MD, MHA, Emergency Medicine, Virginia Mason Medical Center, Seattle, WA. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.