Atelectasis
Partial lung collapse
Atelectasis is the collapse of part or, much less commonly, all of a lung.
Causes
Atelectasis is caused by a blockage of the air passages (bronchus or bronchioles) or by pressure on the outside of the lung.
Atelectasis is not the same as another type of collapsed lung called pneumothorax , which occurs when air escapes from the lung. The air then fills the space outside of the lung, between the lung and chest wall.
Pneumothorax
A collapsed lung occurs when air escapes from the lung. The air then fills the space outside of the lung, between the lung and chest wall. This bui...

Atelectasis is common after surgery or in people who were in the hospital.
Risk factors for developing atelectasis include:
- Anesthesia
- Use of a breathing tube
- Foreign object in the airway (most common in children)
-
Lung diseases
Lung diseases
Lung disease is any problem in the lungs that prevents the lungs from working properly. There are three main types of lung disease:Airway diseases -...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Mucus that plugs the airway
-
Pressure on the lung caused by a buildup of fluid between the ribs and the lungs (called a
pleural effusion
)
Pleural effusion
A pleural effusion is a buildup of fluid between the layers of tissue that line the lungs and chest cavity.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Prolonged bed rest with few changes in position
- Shallow breathing (may be caused by painful breathing)
-
Tumors
that block an airway
Tumors
A tumor is an abnormal growth of body tissue. Tumors can be cancerous (malignant) or noncancerous (benign).
Read Article Now Book Mark Article
Symptoms
Symptoms may include any of the following:
-
Breathing difficulty
Breathing difficulty
Breathing difficulty may involve:Difficult breathingUncomfortable breathingFeeling like you are not getting enough air
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Chest pain
Chest pain
Chest pain is discomfort or pain that you feel anywhere along the front of your body between your neck and upper abdomen.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Cough
Cough
Coughing is an important way to keep your throat and airways clear. But too much coughing may mean you have a disease or disorder. Some coughs are d...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
There are no symptoms if atelectasis is mild.
Exams and Tests
To confirm if you have atelectasis, the following tests will likely be done to view the lungs and airways:
-
Bronchoscopy
Bronchoscopy
Bronchoscopy is a test to view the airways and diagnose lung disease. It may also be used during the treatment of some lung conditions.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Chest CT scan
Chest CT scan
A chest CT (computed tomography) scan is an imaging method that uses x-rays to create cross-sectional pictures of the chest and upper abdomen....
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Chest x-ray
Chest x-ray
A chest x-ray is an x-ray of the chest, lungs, heart, large arteries, ribs, and diaphragm.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Treatment
The goal of treatment is to re-expand the collapsed lung tissue. If fluid is putting pressure on the lung, removing the fluid may allow the lung to expand.
Treatments include one or more of the following:
-
Clap (
percussion
) on the chest to loosen mucus plugs in the airway.
Percussion
Percussion is a method of tapping body parts with fingers, hands, or small instruments as part of a physical examination. It is done to determine:Th...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Deep breathing exercises (with the help of
incentive spirometry devices
).
Incentive spirometry devices
No definition available for this article.
Read Article Now Book Mark Article -
Remove or relieve any blockage in the airways by
bronchoscopy
.
Bronchoscopy
Bronchoscopy is a test to view the airways and diagnose lung disease. It may also be used during the treatment of some lung conditions.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Tilt the person so the head is lower than the chest (called postural drainage). This allows mucus to drain more easily.
- Treat a tumor or other condition.
- Turn the person to lie on the healthy side, allowing the collapsed area of lung to re-expand.
- Use inhaled medicines to open the airway.
- Use other devices that help increase positive pressure in the airways and clear fluids.
Outlook (Prognosis)
In an adult, atelectasis in a small area of the lung is usually not life threatening. The rest of the lung can make up for the collapsed area, bringing in enough oxygen for the body to function.
Large areas of atelectasis may be life threatening, often in a baby or small child, or in someone who has another lung disease or illness.
The collapsed lung usually reinflates slowly if the airway blockage has been removed. Scarring or damage may remain.
The outlook depends on the underlying disease. For example, people with extensive cancer often don't do well, while those with simple atelectasis after surgery have a very good outcome.
Possible Complications
Pneumonia may develop quickly after atelectasis in the affected part of the lung.
Pneumonia
Pneumonia is a breathing (respiratory) condition in which there is an infection of the lung. This article covers community-acquired pneumonia (CAP). ...

When to Contact a Medical Professional
Call your health care provider right away if you develop symptoms of atelectasis.
Prevention
To prevent atelectasis:
- Encourage movement and deep breathing in anyone who is bedridden for long periods.
- Keep small objects out of the reach of young children.
- Maintain deep breathing after anesthesia.
References
O'Donnell AE. Bronchiectasis, atelectasis, cysts, and localized lung disorders. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine . 25th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 90.
Rozenfeld RA. Atelectasis. In: Kliegman RM, Stanton BF, St. Geme JW, Schor NF, eds. Nelson Textbook of Pediatrics . 20th ed. Philadelphia, PA: Elsevier; 2016:chap 408.
-
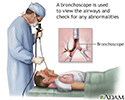
Bronchoscopy - illustration
Bronchoscopy is a surgical technique for viewing the interior of the airways. Using sophisticated flexible fiber optic instruments, surgeons are able to explore the trachea, main stem bronchi, and some of the small bronchi. In children, this procedure may be used to remove foreign objects that have been inhaled. In adults, the procedure is most often used to take samples of (biopsy) suspicious lesions and for culturing specific areas in the lung.
Bronchoscopy
illustration
-
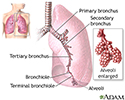
Lungs - illustration
The major features of the lungs include the bronchi, the bronchioles and the alveoli. The alveoli are the microscopic blood vessel-lined sacks in which oxygen and carbon dioxide gas are exchanged.
Lungs
illustration
-
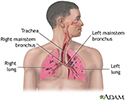
Respiratory system - illustration
Air is breathed in through the nasal passageways, travels through the trachea and bronchi to the lungs.
Respiratory system
illustration
-
Bronchoscopy - illustration
Bronchoscopy is a surgical technique for viewing the interior of the airways. Using sophisticated flexible fiber optic instruments, surgeons are able to explore the trachea, main stem bronchi, and some of the small bronchi. In children, this procedure may be used to remove foreign objects that have been inhaled. In adults, the procedure is most often used to take samples of (biopsy) suspicious lesions and for culturing specific areas in the lung.
Bronchoscopy
illustration
-
Lungs - illustration
The major features of the lungs include the bronchi, the bronchioles and the alveoli. The alveoli are the microscopic blood vessel-lined sacks in which oxygen and carbon dioxide gas are exchanged.
Lungs
illustration
-
Respiratory system - illustration
Air is breathed in through the nasal passageways, travels through the trachea and bronchi to the lungs.
Respiratory system
illustration
Review Date: 8/21/2016
Reviewed By: Denis Hadjiliadis, MD, MHS, Paul F. Harron, Jr. Associate Professor of Medicine, Pulmonary, Allergy, and Critical Care, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.